The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 19, Issue 2 / December 2015
Research Article Pages:64-68
Clinical aspects of benign paroxysmal positional vertigo associated with migraine
Authors: Sertac Yetiser; Meltem Hale Alpsan Gokmen
PDF
Abstract
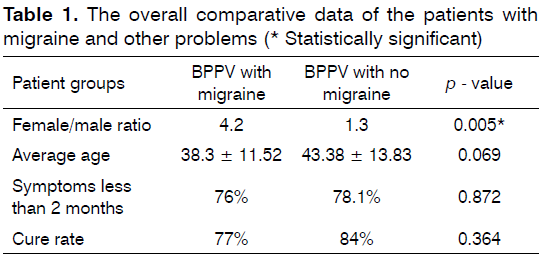
Introduction: Whether clinical features in patients with BPPV and migraine differ from patients with BPPV without migraine is unknown. Objectives: The aim of this study is to compare clinical aspects of patients with or without migraine. Materials and Method: 263 patients with BPPV were enrolled. Patients were investigated in terms of age, gender, symptoms, affected side, type of BPPV and the cure rate. Data were compared in patients with and without migraine. Mean values and standard deviations (± SD) were calculated. One way ANOVA test was used for the analysis. Significance was set at p < 0.005. Results: 32 patients had migraine (11.4%). Gender ratio difference between groups was significant (4.2 vs. 1.3). Comparative analysis of average age between groups was not significant (p = 0.069; 38.50 ± 11.52, 43.38 ± 13.83). Majority of patients had symptoms less than 2 months and the difference was not significant (78.1% vs. 76%). Comparative analysis of cure rate of the therapeutic maneuvers between 2 groups was not significant (77% vs. 84%). Conclusion: Patients with BPPV may have associated migraine. However, this study does not indicate that the presence of migraine is a risk factor for BPPV for the cure since the therapeutic outcome is similar
Keywords: migraine disorders, vertigo, treatment outcome
Introduction
Epidemiological studies suggest co morbidity of migraine and vertigo1. Peripheral and central type of dizziness can be seen in patients with migraine and has been shown to be higher than in the genera [l] population [2,3]. Vestibular migraine is a distinct clinical entity. Vertigo attacks are often separate from headaches and duration of vertigo is not usually within the restrictions of aura [4-6]. Eggers et al.[7] analyzed 228 patients with headache selected from 410 patients with vestibular symptoms and found that those with migraine had distinct vestibular symptoms and presented as recurrent problems. When the dizziness is recurrent in patients with migraine it has a diagnostic and eventually treatment challenge since benign paroxysmal positional vertigo, Ménière’s disease, motion sickness, cerebellar disorders and anxiety syndromes are more frequent in migraineurs than in controls1. Recurrent episodic imbalance is the problem of all age. Idiopathic paroxysmal vertigo of childhood has been defined as a migraine’s equivalent syndrome in which the attacks are brief and sometimes may mimic other problems [8].
Pathophysiological mechanism which induces the sense of vertigo in patients with BPPV is well documented[9]. Freely floating otoconia inside the semicircular canals or those adhering to the cupula can provoke nystagmus and vestibular disturbance during sudden head motion [10]. The origin of these deposits is claimed to be due to degeneration in utricular neuroepithelium, the incidence of which increases mostly with trauma, ischemia and vascular damage. Roberts et al.[11] presented a patient with cupulolithiasis variant of horizontal canal BPPV who did not benefit from several attempts of liberatory maneuvers, but the patient got well after migraine therapy which raised a question of differential diagnosis and the possibility of co-incidence.Could migraine and BPPV share common pathological basis in patients with positional vertigo? If this is the case, do the clinical features in patients with BPPV and migraine differ from patients with BPPV without migraine? The clinical aspect of patients with BPPV and migraine has not been completely clarified. Demographic analysis of patients with BPPV has been studied before which indicates an associated migraine in some patients[12]. However, comparative analysis of clinical aspects in those patients with or without migraine has never been accomplished before. The aim of this study is to particularly analyze the clinical aspects of patients with BPPV and migraine and compare with those having no migraine.
Material abd Methods
Two hundred and sixty-three patients with BPPV confirmed by videonystagmography (VNG) (Micromed, Inc, USA) who have been evaluated between 2009-2014 during outpatient clinical visit were enrolled in the study. All authors have full access to the study data. A verbal and a signed informed consent were obtained from each patient. The procedures were in accordance with the ethical standards of the declaration of Helsinki and of the institutional review board. Distribution of gender, age and affected side were reviewed. Associated problems were noted. Those who have no clear event-related problem (especially trauma) were accepted as “idiopathic”. Patients were grouped as those with posterior canal BPPV (PC-BPPV), lateral canal BPPV (LC-BPPV), whether cupulolithiasis or canalolithiasis, and superior canal BPPV (SC-BPPV). Patients were grouped as those with or without migraine. Diagnosis and classification of migraine and its differentiation from other type of headaches was based on third edition of International classification of headache disorders (ICHD-III beta) by international headache society (IHS)[13]. These criteria were also applied to those whose records were before 2013. All patients with migraine had migrainous headache with or without aura and they all were diagnosed in our institution and followed by our neurology staff. Second group of patients contained those without migraine. Patients were also grouped according to the duration of BPPV symptoms. A 2-months period was decided as an artificial cut-off point at the initial diagnosis of patients with BPPV in grouping them as those with the duration of symptoms less than or more than 2 months.
Diagnosis of LC-BPPV with canalolithiasis or cupulolithiasis was based on medical history and the presence of geotropic or apogeotropic nystagmus (bidirectional, horizontal) during roll-on maneuver. Affected side for LC-BPPV was determined according to the severity of nystagmus as seen on VNG recording which was severe on the affected side in patients with geotropic nystagmus and was severe on the healthy side in patients with apogeotropic nystagmus. Diagnosis of PC-BPPV was based on medical history and the presence of clockwise or counter-clockwise rotatory nystagmus (torsional, up-beating) during head-hanging maneuver. Diagnosis of SC-BPPV was based on medical history and the presence of clockwise or counter-clockwise rotatory nystagmus (torsional, down-beating) during the headhanging maneuver. Patients with PC-BPPV were treated with Epley maneuver. Patients with SC-BPPV were treated with Li or reverse Epley maneuver. Patients with LC apogeotropic or geotropic nystagmus were treated with Barbeque, Semont’s or Gufoni maneuvers. The involved side was reassured according to the patient sense of disturbance or lying down positioning test [14]. All patients were re-evaluated at maximum 7 days. Mean values and standard deviations (± SD) were calculated. One way ANOVA test was used for multiple variance analysis of the groups. (Statistical Package for the Social Sciences 17.0 version, IBM, Chicago, III, USA). Statistical significance was set at p < 0.05.
Results
There were 104 men and 159 women. Age was ranging between 10 and 84 (42.76 ± 13.54). One hundred and eleven patients had right-sided (41.4%), 120 patients had left-sided problem (45.6%). It was not possible to identify the effected side due to multiple canal involvement or in some patients with LC-BPPV due to equal severity of nystagmus on both sides in 32 patients. One hundred and twenty patients had PC-BPPV, 38 patients had LC-cupulolithiasis, 60 patients had LCcanalolithiasis, 9 patients had SC-BPPV and 25 patients had nystagmus in both Dix-Hallpike and roll-on maneuvers (either multiple canal involvement or technical problems). Eleven patients had nystagmus on both sides during Dix- Hallpike maneuver. One hundred and forty-seven patients were defined as “idiopathic” since they don’t have any associated or event-related problem (55.8%). Thirty-two patients had migraine (11.4%). Nineteen patients had an evident story of trauma, even if it is minor, within a few weeks prior to symptoms (dental surgery, mountain biking, skate-roller in amusement park, intense physical activity etc.) (7.2%). 10 patients had vestibular neurinitis prior to BPPV, 5 patients had Ménière’s disease and 3 patients had otosclerosis (6.8%). Goiter, hypertension, high cholesterol, diabetes, gastric ulcer, osteoarthritis, cancer (lymphoma, thyroid and breast cancers etc), chronic coronary and lung problems were the other miscellaneous problems (22.6%) (information provided by the patients). There were 231 patients (98 males and 133 females) without migraine (gender ratio;1:1.3). The age at first manifestation of BPPV was ranging between 14 and 84 (43.38 ± 13.83). 87 patients had LC-BPPV (87/231; 37.7%), 103 patients had PC-BPPV (103/231; 44.6%), eight patients had SC-BPPV (8/231; 3.4%), 33 patients had multiple canal involvement/stimulation (33/231; 14.3%). Fifty-five patients having BPPV without migraine had symptoms longer than 2 months (55/231; 24%) and 176 patients had symptoms less than 2 months (176/231; 76%).
There were 6 males (6/32; 18.7%) and 26 females (26/32; 81.3%) with migraine (1:4.2). The number of women with BPPV and migraine was higher than that of men. Comparative analysis of average gender ratio between BPPV with migraine and BPPV without migraine was statistically significant (1.3 vs. 4.2, p < 0.005). The age was ranging between 10 and 69. Average age was lower in 32 patients with BPPV and migraine as compared to 231 patients with other BPPV group. However, the difference was not statistically significant. (p = 0.069; 38.50 ± 11.52, 43.38 ± 13.83). Eleven patients had LCBPPV (11/32; 34%), 17 patients had PC-BPPV (17/32; 53%), one patient had SC-BPPV (1/32; 3%), 3 patients had multiple canal involvement (3/32; 10%). Comparative analysis of frequency of leading BPPV problem (PCBPPV) between BPPV with migraine and BPPV without migraine was not statistically significant (45.2% vs. 44.6%). Seven patients having BPPV with migraine had symptoms longer than 2 months (7/32; 21.9%) and 25 patients had symptoms less than 2 months (25/32; 78.1%). Comparative analysis of average symptom duration between BPPV with migraine and BPPV without migraine for patients with symptoms less than 2 months was not statistically significant (76% vs. 78.1%, p = 0.872). The overall cure rate after one single maneuver was 82%. Comparative analysis of cure rate between BPPV with migraine and BPPV without migraine was not statistically significant (77% vs. 84%, p = 0.364). Relevant comparative data are presented on Table 1.
Discussion
Very few studies have been published so far about co-existence of migraine and BPPV. Ishiyama et al.[15] studied 247 patients with BPPV and found that history of migraine was 3 times more common in patients with idiopathic BPPV than in those who developed it after head trauma or surgery. Von Brevern et al.[16] performed a population based study of patients with dizziness using the criteria of BPPV. The odds ratio of migraine in their BPPV group versus control was 7.5. Uneri reviewed 476 patients with PC-BPPV and found that migraine (54.8%) was more common in patients with BPPV than in general population[17]. The incidence of migraine in patients with BPPV in this series (11.4%) is lower than those reported in other studies, but it is more common than those who had event-related trauma story. Epidemiological studies suggest that migraine is more common in females than in males. Gender specific evaluation in this series also demonstrated significantly higher proportion of association of migraine and BPPV in women. The most common BPPV form was idiopathic (55.8%) in which a clear cause could not be identified. Majority of patients had BPPV symptoms less than 2 months (76%). But, that long-term follow-up is necessary to understand the frequency of recurrence and to clarify any causative factor particularly in those with unknown etiology. On the other hand, patients who have been enrolled for the study were from the same medical center. Some limitations may also exist to rise a general conclusion from a single center study.
In clinical practice, episodic vertigo presents diagnostic and therapeutic problems. The leading causes of recurrent attacks of vertigo are Ménière’s disease, BPPV, vestibular migraine, vestibular paroxysmal, vertebra-basilar ischemia, orthostatic hypotension, panic attacks etc. Clinical recognition of vestibular migraine has still lack of some consensus because of discussions about the validity of the standard diagnostic criteria. However, the diagnosis is particularly based on recurrent vestibular symptoms, a history of migraine and exclusion of other causes of vestibular symptoms. Duration of acute episodes is limited to 5 minutes to 72 hours with moderate or severe intensity. Symptoms that qualify for a diagnosis of vestibular migraine include various types of vertigo. Because the headache is often absent during acute attacks, motion sickness, positional or head-induced type of vertigo in migraine may present a diagnostic challenge with true BPPV[4,11]. Resolution of vestibular symptoms with anti-migraine drugs in patients with migraine-related vertigo as well as a need to initiate preventive therapy provides a challenge for the clinician for the differential diagnosis. One should focus on migraine especially for BPPV patients who had no relief of symptoms after several attempts of liberatory maneuvers.
The possible common pathophysiological mechanism of BPPV and migraine may relate to degenerating vestibular neuroepithelium. Migraine cannot be considered only a central phenomenon which selectively targets the inner ear in some instances[18]. Episodic vasospasm can lead to hypo perfusion of the peripheral vestibular system and subsequent damage. Radtke et al.[19] have followed 61 patients with definite vestibular migraine and have found that 15% of initial concomitant cochlear symptoms have risen to 49% during follow-up. In a multi-variant epidemiological study, Lempert et al.[20] have found that age, hyperlipidemia, hypertension and migraine represent risk factor for BPPV but they did not find any association between BPPV and other well established risk factors like diabetes, obesity and smoking. Pathophysiological link between BPPV and migraine is not clear but it may be related to ischemic damage to otolithic organ. On the other hand, the effect of presence of migraine on symptomatic relief of therapeutic maneuvers in patients with BPPV has not been clarified so far since the comparative studies were lacking.
In conclusion, this study is in accordance with 3 previous studies that patients with BPPV may have associated migraine which has to be included in diagnostic issues as well as treatment plan[15,17,20]. BPPV associated with migraine was more common in female population. The cure rate of therapeutic maneuvers in patients with migraine and BPPV was not statistically significant but lower as compared those without migraine. Our study does not indicate that the presence of migraine is a risk factor for BPPV for the cure since the therapeutic outcome is similar.
Acknowledgments
Authors would like to thank to all personnel of the department for their valuable help to the patients.
This study was registered to www.clinicaltrials.gov (NCT02615314)
References
- Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol. 2009;256(3):333-8. DOI: http://dx.doi.org/10.1007/s00415-009-0149-2
- Cass SP, Furman JM, Ankerstjerne K, Balaban C, Yetiser S, Aydogan B. Migraine-related vestibulopathy. Ann OtolRhinolLaryngol. 1997;106(3):182-9. PMID: 9078929 DOI: http://dx.doi.org/10.1177/000348949710600302
- Lee H, Sohn SI, Jung DK, Cho YW, Lim JG, Yi SD, et al. Migraine and isolated recurrent vertigo of unknown cause. Neurol Res. 2002;24(7):663-5. DOI: http://dx.doi.org/10.1179/016164102101200726
- Neuhauser H, Lempert T. Vertigo and dizziness related to migraine: a diagnostic challenge. Cephalalgia. 2004;24(2):83-91. DOI: http://dx.doi.org/10.1111/j.1468-2982.2004.00662.x
- Dieterich M, Brandt T Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol. 1999;246(10):883-92.
- Brantberg K, Trees N, Baloh RW. Migraine-associated vertigo. ActaOtolaryngol. 2005;125(3):276-9. PMID: 15966697 DOI: http://dx.doi.org/10.1080/00016480510003165
- Eggers SD, Staab JP, Neff BA, Goulson AM, Carlson ML, Shepard N.T Investigation of the coherence of definite and probable vestibular migraine as distinct clinical entities. OtolNeurotol. 2011;32(7):1144-51. DOI: http://dx.doi.org/10.1097/MAO.0b013e31822a1c67
- Marcelli V, Piazza F, Pisani F, Marciano E. Neuro-otological features of benign paroxysmal vertigo and benign paroxysmal positioning vertigo in children: a follow-up study. Brain Dev. 2006;28(2):80-4. DOI: http://dx.doi.org/10.1016/j.braindev.2005.05.003
- Gacek RR. Pathology of benign paroxysmal positional vertigo revisited. Ann OtolRhinolLaryngol. 2003;112(7):574-82. PMID: 12903676 DOI: http://dx.doi.org/10.1177/000348940311200702
- Parnes LS, McClure JA. Free-floating endolymph particles: a new operative finding during posterior semicircular canal occlusion. Laryngoscope. 1992;102(9):988-92. PMID: 1518363
- Roberts RA, Gans RE, Kastner AH. Differentiation of migrainous positional vertigo (MPV) from horizontal canal benign paroxysmal positional vertigo (HC-BPPV). Int J Audiol. 2006;45(4):224-6. PMID: 16684703 DOI: http://dx.doi.org/10.1080/14992020500429658
- Yetiser S, Ince D. Demographic analysis of benign paroxysmal positional vertigo as a common public health problem. Ann Med Health Sci Res. 2015;5(1):50-3. DOI: http://dx.doi.org/10.4103/2141-9248.149788
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629-808. DOI: http://dx.doi.org/10.1177/0333102413485658
- Yetiser S, Ince D. Diagnostic Role of Head-Bending and Lying-Down Tests in Lateral Canal Benign Paroxysmal Positional Vertigo. OtolNeurotol. 2015;36(7):1231-7. DOI: http://dx.doi.org/10.1097/MAO.0000000000000774
- Ishiyama A, Jacobson KM, Baloh RW. Migraine and benign positional vertigo. Ann OtolRhinolLaryngol. 2000;109(4):377-80. PMID: 10778892 DOI: http://dx.doi.org/10.1177/000348940010900407
- von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J NeurolNeurosurg Psychiatry. 2007;78(7):710-5. PMID: 17135456 DOI: http://dx.doi.org/10.1136/ jnnp.2006.100420
- Uneri A. Migraine and benign paroxysmal positional vertigo: an outcome study of 476 patients. Ear Nose Throat J. 2004;83(12):814-5. PMID: 15724736
- Battista RA. Audiometric findings of patients with migraine-associated dizziness. OtolNeurotol. 2004;25(6):987-92. DOI: http://dx.doi.org/10.1097/00129492-200411000-00021
- Radtke A, von Brevern M, Neuhauser H, Hottenrott T, Lempert T. Vestibular migraine: long-term follow-up of clinical symptoms and vestibulo-cochlear findings. Neurology. 2012;79(15):1607-14. PMID: 23019266 DOI: http://dx.doi.org/10.1212/WNL.0b013e31826e264f
- Lempert T, Leopold M, von Brevern M, Neuhauser H. Migraine and benign positional vertigo. Ann OtolRhinolLaryngol. 2000;109(12 Pt 1):1176.
References
Dept of Neurology - Anadolu Medical Center - Kocaeli - AC - Turkey. E-mail: syetiser@yahoo.com / hale.gokmen@anadolusaglik.org
Institution: Anadolu Medical Center, Gebze - Kocaeli
Send correspondence to:
Sertaç Yetiser
Dept of Neurology
Anadolu Medical Center - Kocaeli - AC - Turkey
E-mail: syetiser@yahoo.com
Paper submitted to the RBCMS-SGP (Publishing Management System) on November 27, 2015; and accepted on December 2, 2015. cod. 218
Citation: Yetiser S, Gokmen MHA. Clinical aspects of benign paroxysmal positional vertigo associated with migraine. Int Tinnitus J. 2015;19(2):64-68