The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 21, Issue 1 / June 2017
Research Paper Pages:2-6
Cochlear implantation improves hearing and vertigo in patients after removal of vestibular schwannoma
Authors: Ariane Roemer, Thomas Lenarz, Anke Lesinski-Schiedat
PDF
Abstract
Objective: With rising quality of speech perception in cochlear implant users, the indication widens. Nowadays, cochlear implantation is reasonable even in vestibular schwannoma patients. Speech perception with a cochlear implant is in these patients as promising as in patients with sensorineural hearing loss. However, the impact of cochlear implantation on vertigo and tinnitus after removal of vestibular schwannoma has not been investigated yet. Methods: In a retrospective study, we analysed 12 patients treated with a cochlear implant after removal of vestibular schwannoma. Results: In addition to a promising hearing perception - all patients reported improvement of vertigo. This improvement was also demonstrated by postural analysis. Improvement of tinnitus was achieved in 50% of the patients. Conclusion: Cochlear implantation seems a promising treatment for hearing loss, vertigo and even tinnitus in patients after removal of vestibular schwannoma. However, for successful cochlear implantation with adequate speech perception and improvement of vertigo and tinnitus, functional hearing nerve and intact inner ear anatomy is necessary.
Keywords: cochlear implantation, vestibular schwannoma, vertigo, tinnitus
Introduction
Vestibular schwannomas (VSs) are the most common [1-4] intracranial schwannomas with an annual incidence of 1 per 100,000 [2-4]. They originate from the Schwann cells of the vestibular portion of the 8th cranial nerve. They are benign generally slow growing tumours with a wide variability in size and growth rate. First described by Mr. Sandiford in 1777 as a single case, presented in 1830 as a relevant clinical issue, the first removal was performed in 1892 by Sir C. Ballance [5]. At this time, the mortality rate was over 80%. Depending on the symptoms and the location of the tumour, following treatment options are available nowadays: observation, stereotactic radiosurgery, fractionated radiotherapy, and microsurgery. Surgical approaches include the translabyrinthine, the retrosigmoid/suboccipirtal and the middel fossa approach and the mortality rate is lower than 2% [6]. Due to incidental diagnosis of asymptomatic lesions after widespread use of MRI, the incidence appears to be increasing [7].
The aetiology of vestibular schwannomas is widely unknown, whereas in neurofibromatosis a polyclonal origin is suspected [8]. Neurofibromatosis type is a hereditary disease associated with VS. In Type I Neurofibromatosis, 90% of the patients develop at least one-sided VS. Ten times less frequent is the neurofibromatosis type 2 which is associated with bilateral VSs in 90% of the affected patients [2,9]. Considering the large number of the affected patients, early diagnosis and treatment of the disease is mandatory in order to achieve favourable results. However, the chances to preserve hearing decrease with increasing tumour size despite advanced surgical techniques and a high percentage of the patients experience severe to profound hearing loss [10-13]. Therefore, the demand for a sufficient hearing supply after surgical removal is rising. The quantity and quality of hearing rehabilitation is increasing from normal hearing aids, cross- and bicross- hearing-systems, bone conducted hearing aids, middle ear implants (MOI), cochlear implantation (CI), auditory brainstem implant (ABI) and auditory midbrain implant (AMI). After surgical removal of VSs, especially in neurofibromatosis type 2 patients, the supply with ABI is in most cases an option, but several studies showed an unsatisfactory outcome [8,11,13,14]. Especially the speech perception with an ABI in adults [15], compared to the supply in young children [16], is a huge breakdown. In an increasing number of patients, the auditory nerve can be anatomically preserved despite extensive surgical removal of the schwannoma. Therefore, more and more CIs are an option for the treatment of hearing loss for these patients. Several studies suggest a very good hearing rehabilitation of acoustic neuroma patients after CI [9,17,18]. However, nearly all studies are limited due to small patient numbers [19,20] - reporting case files or groups of up to 3 patients. Another shortcoming of the studies reported in the literature is the lack of information on improvements regarding impairments associated with an acoustic neuroma, for example tinnitus and vertigo. The purpose of this paper is the retrospective analysis of the impact of CI on hearing improvement as well as the improvement of vertigo and tinnitus in patients implanted after surgical removal of VS.
Materials and Methods
Patients
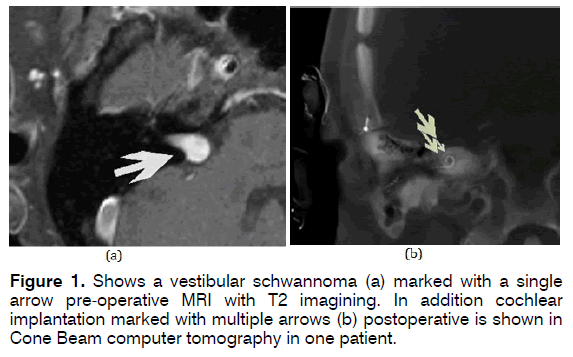
In this retrospective study, we analysed 12 adults (8 men and 4 women, mean age of 45,58 year ranging from 35 to 80 years at date of cochlear implantation) treated with a CI for hearing improvement after surgical removal of VS (Figure 1a). Among these, two patients suffered from neurofibromatosis type 2 with unilateral VS. A surgical removal of VS was performed in all patients between 1988 and 2013. The removal of the VS was performed at other clinics in 4 patients. The remaining patients were treated in our Centre with retrosigmoid and middle fossa approach. Included were all patients who received vestibular schwannoma operation and cochlear implantation in a second setting on the same side. Exclusion criteria were revision operations, implantation with AMI or ABI as well as patients under 18 year of age.
Implantations
All cochlear implantations were performed in our clinic by experienced surgeons according to standard operation procedures without complications (4 operations on the left side, 8 on the right side) during the period of 2005 until 2014. The standard procedure involves a retroauricular approach, mastoidectomy, posterior tympanotomy and cochleostomy. To ensure a correct electrode function, the electrodes were tested before and immediately after insertion, as well as at the second postoperative day.
The proper postoperative function and electrode position was demonstrated electrophysiologically as well as radiologically via cone beam CT (Figure 1b).
The following implants were chosen by the patients:
• Advanced Bionics HiRes 90K electrode (1 patient)
• Cochlear nucleus CI 422 (2 patients)
• Cochlear nucleus CI 512 (3 patients)
• Cochlear nucleus freedom (1 patient)
• Cochlear nucleus contour advanced (2 patients)
• Cochlear nucleus RE 24 (3 patients)
All electrodes are not considered as hearing preserving and cover all frequencies. All patients received the first fitting of the CI 5-7 weeks after operation during a 5-day in-patient treatment with daily fine tuning and pedagogic therapy as an introduction to daily individual training. We had limited access to preoperative symptoms (hearing loss, vertigo, and tinnitus) and audiologic results before surgical removal of VS in 4 patients due to the fact that they were treated on their vestibular schwannoma at other clinics. However, symptoms such as hearing loss, vertigo and tinnitus occurring prior to and after implantation were extracted from the charts of the patients. As we want to demonstrate the effects of cochlear implantation after vestibular schwannoma operation, for this study the functional test prior to vestibular schwannoma surgery are not relevant.
Functional tests
A caloric test was performed for the functional evaluation of the vestibular nerve prior to surgical removal of the VS. In addition, patients received caloric tests and dynamic prosturography (SMART EquiTest®) as a preparation for cochlea implantation. The speech perception was tested with the German monosyllable “Freiburg Einsilber-Test“ in soundproof conditions. All test were additionally performed 5-7 weeks postoperative after activation of the implant. Statistical comparisons were done by 2 × 2 contingency table, chi-square statistics and One-Way ANOVA. Statistical significance was assumed at p < 0.05 without corrections for multiple testing.
Results
After surgical removal, 11 patients showed a total hearing loss at the side of the VS. One showed a typical severe hearing loss in the high frequencies with residual hearing in the lower frequencies without a benefit in speech perception. Despite unilateral VS and the surgery associated with for treatment, three (25%) from the 12 patients presented a bilateral profound hearing loss. All other patients had normal hearing on the untreated side.
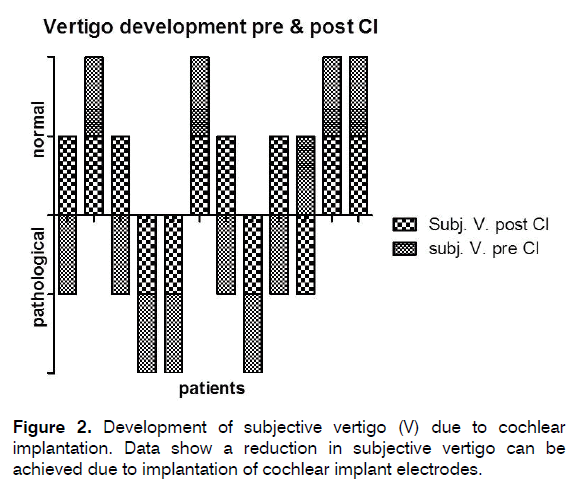
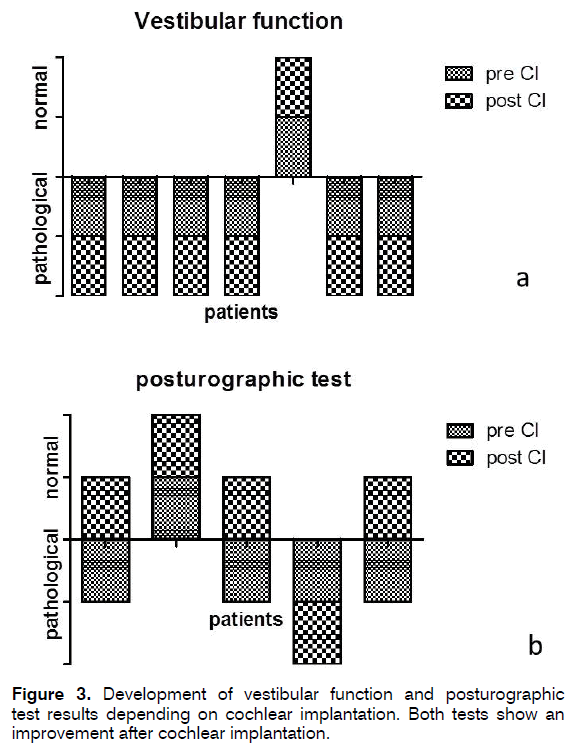
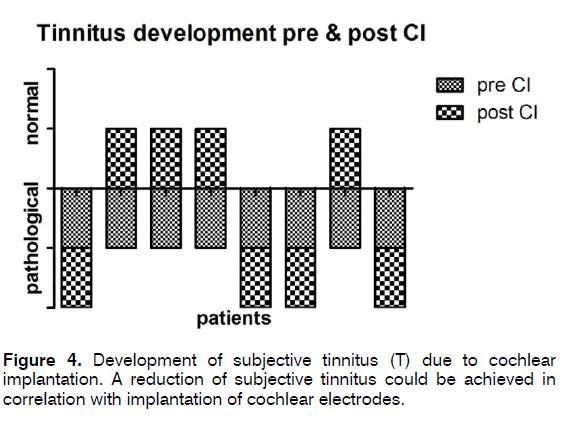
7 of the 12 (58%) patients complained about dizziness prior to CI. Out of these, 4 (57%) patients showed improvement of dizziness and 3 (43%) remained idem (Figure 2). Of the 5 patients without any dizziness complaints pre CI, 4 (80%) remained free of dizziness and 1 (20%) developed vertigo 4 month after implantation. Figures 2 and 3 show the subjective and objective examination for dizziness. Objectively testing the vestibular function, we detected a vestibular deficit prior to cochlea implantation in 11 patients (Data not shown). From these 11 only 7 agreed with a postoperative vestibular testing (Figure 3a). Here all patients showed equal test results. Consequently, 1 (9%) person had a normal vestibular function. This patient preserved this function also after cochlea implantation. The six patients with pathological vestibular tests also agreed to posturography (Figure 3b). Among these, 3 (27%) patients had a compensated loss of vestibular function in posturography (Figure 3b). Tinnitus was described by 8 patients prior to cochlea implantation and only these were depicted in Figure 4. After implantation, the same 8 patients described a persistent tinnitus, but 4 (50%) out of these 8 patients expressed an explicit improvement within loudness of the tinnitus and daily masking possibilities. Three (75%) out of these 4 patients also experienced improvement of vertigo after cochlea implantation. Using Chi-Square and One- Way-ANOVA - due to small test number- we could achieve no statistical significance. A speech perception from 52% to 85% could be achieved and therefore expresses the average outcome for our implanted patients [21].
Discussion
Development of cochlea implants rises fast, while its way from its beginning in the 18th century till now was rough [22-24]. Because of the tremendous success in speech understanding, the indication for a CI is widened. Especially in seniors, CIs become more important to enable better speech understanding and to include them therewith in the social environment [25]. It is also discussed whether better hearing can diminish dementia [26,27]. Beside improvement of speech understanding and therefore communication, the balance system plays an important role in the rehabilitation especially of older patients [27-29]. Because the inner ear function includes also the labyrinthine, this has to be observed carefully while defining the indication to CI surgery and has to be monitored after surgery. Beside this, a tinnitus - as a further source of stress - can disguise the subjective impression of a successful speech rehabilitation. One has to consider that vertigo and tinnitus are the most frequent complains after acoustic neuroma extirpation. Grauvogel et al. described a huge loss of quality of life due to the presence of these two symptoms [30]. Thus, a reduction of complains and therefore a rise in life quality should be the goal of each ENT surgeon.
In our study, 57% of our patients with vertigo showed a subjective substantial improvement. In other studies the percentage of patients with persistent vertigo after VS surgery varies between 9 and 60% [31]. We therefore present an average vertigo expression in our patients. The duration between vestibular schwannoma operation and cochlear implantation was at least 8 month. Therefor a spontaneous recovery after vestibular schwannoma can be neglected.
In addition, we could show that the subjective improvement of the vertigo was only partly reflected by the results of the objective vestibular tests performed.Besides the detection of a damage of an intact vestibular system through cochlear implantation, vestibular function tests were also used to determine any changes of restricted vestibular function. Thus, cochlear implantation seems not to be associated with an increased risk for loss of vestibular function. However, one has to consider that this was a very special patient collective with only a small number of patients included.
The posturography (Equi® test) helps to identify the compensation of vertigo. We could verify that, of the 4 patients with uncompensated vertigo, three developed a good compensation after cochlear implantation. This confirms the interaction of auditory stimulation and vertigo suppression corroborating the findings of Schutt et al. [19] and underlining the significance of hearing in spatial orientation.
Improvement of the loudness, frequency and intensity of the tinnitus was expressed by 50% of the patients and the ability to conceal the tinnitus was emphasized – supporting previous findings [32]. Never the less, this percentage is under the expected improvement in unilaterally implanted deaf people without vestibular schwannoma operation [33]. This difference may be due to the small numbers of patients included in our study due to small number of patients receiving cochlear implantation after vestibular schwannoma removal. However, one drawback in the present study is the lack of evaluation of impairment associated with tinnitus, e.g., by the use of tinnitus questionnaires. Since tinnitus is one of the main symptoms in patients with VS, the aetiology here is most likely neural damage due to compression via the tumour. Considering the aetiologies of tinnitus in deaf or hearing impaired people, the etiologic is mainly idiopathic. This cannot be seen in the ethology of the tinnitus in our cases, as the tinnitus most likely result from a neural trauma due to compression by the tumour. We therefore assume a regression in tinnitus due to the constant stimulation of the traumatic neurons. It has been shown before that loss of stimulation leads to a degeneration of neurons. New stimulation leads to spreading of neurites and reactivation of the neuron. Tinnitus can be assumed as a mislead information from degenerated neurons. These misinformation could be reduced before via electrical stimulation, also without clear acoustic stimulation. Heerman et al. could show that cochlear implanted patients will even report a suppression of tinnitus with subliminal stimulation [34].
Interestingly, 75% of the patients showing a tinnitus improvement also show improvement in vertigo. This connection was not described before and leads us to new questions about the physiology of the hearing-balancesystem. We assume reduced compensatory mechanisms in the balance system caused by trauma of the vestibular and cochlea nerves with resulting deafness and tinnitus. As the central vestibular function is wide spread [35], a direct correlation has not been found yet. In addition, a participation of the limbic system or psychological factors may be responsible for an interconnection between improved vertigo and reduced tinnitus. Furthermore it could be shown that tinnitus as well as vertigo reduction is highly decreased in patients describe a decrease in stress due to the improved hearing. Psychological factors therefore seem to play an important role in vertigo and tinnitus in cochlear implant patients.
In summary, all patients showed good speech perception comparable to cochlea implant users without history of VS. Furthermore, there is a significant improvement in tinnitus and vertigo due to cochlea implantation after extirpation of VS. Thus, we here provide first hint that CI may be an ideal adjuvant treatment not only for HL but also for vertigo and tinnitus in patients with surgical removed vestibular schwannoma. However, further investigations are necessary to judge the effect of CI in vertigo and tinnitus in VS patients. A prospective controlled multicentre study with standardized subjective and objective analysis is here mandatory.
References
- Ganesan P, Sankaran P, Kothandaraman PP. A rare case of hearing impairment due to cerebello-pontine angle lesion: trigeminal schwannoma. J Int Adv Otol. 2015;11:170-2.
- Evans DGR, Moran A, King A, Saeed S, Gurusinghe N, Ramsden R. Incidence of vestibular schwannoma and neurofibromatosis 2 in the North West of England over a 10-year period: higher incidence than previously thought. Otol Neurotol. 2005;26:93-7.
- Stangerup SE, Tos M, Thomsen J, Caye-Thomasen P. True incidence of vestibular schwannoma? Neurosurgery. 2010;67:1335-40.
- Tos M, Thomsen J. Epidemiology of acoustic neuromas. J Laryngol Otol. 1984;98:685-92.
- Schwager K. Acoustic neuroma/vestibular schwannoma. HNO. 2011;59:7-8.
- Mura J, Cuevas JL, Rojas-Zalazar D, Riquelme F, Luna F, Sariego H, et al. Schwannomas vestibulares: experiencia en el tratamiento quirúrgico de 67 casos en 10 anos. Neurocirugia. 2015;26:261-7.
- Lin D, Hegarty JL, Fischbein NJ, Jackler RK. The prevalence of “incidental” acoustic neuroma. Arch Otolaryngol Head Neck Surg. 2005;131:241-4.
- Lenarz T, Moshrefi M, Matthies C, Frohne C, Lesinski-Schiedat A, Illg A, et al. Auditory brainstem implant: part I. Auditory performance and its evolution over time. Otol Neurotol. 2001;22:823-33.
- Neff BA, Wiet RM, Lasak JM, Cohen NL, Pillsbury HC, Ramsden RT, et al. Cochlear implantation in the neurofibromatosis type 2 patient: Long-term follow-up. Laryngoscope. 2007;117:1069-72.
- Kronenberg J, Horowitz Z, Hildesheimer M. Intracochlear schwannoma and cochlear implantation. Ann Otol Rhinol Laryngol. 1999;108:659-60.
- Merkus P, Di Lella F, Di Trapani G, Pasanisi E, Beltrame MA, Zanetti D, et al. Indications and contraindications of auditory brainstem implants: Systematic review and illustrative cases. Eur Arch Oto-Rhino-Laryngology. 2014; 271:3-13.
- Matthies C, Brill S, Kaga K, Morita A, Kumakawa K, Skarzynski H, et al. Auditory brainstem implantation improves speech recognition in neurofibromatosis type II patients. ORL J Otorhinolaryngol Relat Spec. 2013;75:282-95.
- Matthies C, Brill S, Varallyay C, Solymosi L, Gelbrich G, Roosen K, et al. Auditory brainstem implants in neurofibromatosis Type 2: is open speech perception feasible? J Neurosurg. 2014;120:546-58.
- Goffi-Gomez MVS, Magalhães AT, Brito Neto R, Tsuji RK, Gomes MDQT, Ferreira Bento R. Auditory brainstem implant outcomes and MAP parameters: Report of experiences in adults and children. Int J Pediatr Otorhinolaryngol. 2012;76:257-64.
- McKay CM, Azadpour M, Jayewardene-Aston D, O’Driscoll M, El-Deredy W. Electrode Selection and Speech Understanding in Patients With Auditory Brainstem Implants. Ear Hear. 2015;36:45-63.
- Colletti L, Shannon R V., Colletti V. The Development of Auditory Perception in Children after Auditory Brainstem Implantation. Audiol Neurotol. 2014;19:386-94.
- Garin P, Deggouj N, Decat M, Gersdorff M. Vestibular schwannoma and cochlear implantation. Cochlear Implants Int. 2005;6:28-31.
- Ahsan S, Telischi F, Hodges A, Balkany T. Cochlear Implantation Concurrent with Translabyrinthine Acoustic Neuroma Resection. Laryngoscope. 2003;113:472-74.
- Schutt CA, Kveton JF. Cochlear implantation after resection of an intralabyrinthine schwannoma. Am J Otolaryngol. 2014;35:257-60.
- Tono T, Ushisako Y, Morimitsu T. Cochlear implantation in an intralabyrinthine acoustic neuroma patient after resection of an intracanalicular tumour. J Laryngol Otol. 1996;110:570-73.
- Illg a, Bojanowicz M, Lesinski-Schiedat A, Lenarz T, Büchner A. Evaluation of the Bimodal benefit in a large cohort of cochlear implant subjects using a contralateral hearing aid. Otol Neurotol. 2014;35:e240-4.
- Mudry A, Mills M. The early history of the cochlear implant. JAMA Otolaryngol Head Neck Surg. 2013;139:446-53.
- O’Donoghue G. Cochlear Implants -Science, Serendipity, and Success. N Engl J Med. 2013;369:1190-93.
- Ramsden RT. History of cochlear implantation. Cochlear Implants Int. 2013;14:S3-5.
- Lenarz M, Sönmez H, Joseph G, Büchner A, Lenarz T. Cochlear implant performance in geriatric patients. Laryngoscope. 2012;122:1361-65.
- Modest MC, Carlson ML, Wanna GB, Driscoll CL. Cochlear Implantation in Patients With Superficial Siderosis : Seven Cases and Systematic Review of the Literature. Otol Neurotol. 2015; 36:1191-96.
- Martini A, Castiglione A, Bovo R, Vallesi A, Gabelli C. Aging, cognitive load, dementia and hearing loss. Audiol Neurotol. 2015;19:2-5.
- Lee JH. Cochlear implantation in the elderly. J Korean Med Assoc. 2011;54:925-34.
- Yin M, Ishikawa K, Wong WH, Shibata Y. A clinical epidemiological study in 2169 patients with vertigo. Auris Nasus Larynx. 2009;36:30-5.
- Grauvogel J, Kaminsky J, Rosahl SK. The impact of tinnitus and vertigo on patient-perceived quality of life after cerebellopontine angle surgery. Neurosurgery. 2010; 67:601-9.
- Swan IR. Is early management of acoustic neuroma important? J R Soc Med. 2000;93:614-7.
- Buechner A, Brendel M, Lesinski-Schiedat A, Wenzel G, Frohne-Buechner C, Jaeger B, et al. Cochlear implantation in unilateral deaf subjects associated with ipsilateral tinnitus. Otol Neurotol. 2010;31:1381-85.
- Blasco MA, Redleaf MI. Cochlear implantation in unilateral sudden deafness improves tinnitus and speech comprehension. Otol Neurotol. 2014;35:1426-32.
- Battmer RD, Heermann R, Laszig R. Suppression of tinnitus by electric stimulation in cochlear implant patients. HNO. 1989;37:148-52.
- Bottini G, Sterzi R, Paulesu E, Vallar G, Cappa SF, Erminio F, et al. Identification of the central vestibular projections in man: a positron emission tomography activation study. Exp Brain Res. 1994;99:164-69.
References
Hannover Medical School, ENT department, Carl-Neuberg-Straßee 1, 30171 Hannover, Germany, E-mail: roemer.ariane@mh-hannover.de/ /lenarz.thomas@mh-hannover.de/les@hoerzentrum-hannover.de
Institution: Hannover Medical School, Germany
Send correspondence to:
Ariane Roemer
Hannover Medical School, ENT department, Carl-Neuberg-Straßee 1, 30171 Hannover, Germany. E-mail: roemer.ariane@mh-hannover.de
Paper submitted to the ITJ-EM (Editorial Manager System) on November 16, 2017; and accepted on January 10, 2017.
Citation: Roemer A, Lenarz T, Lesinski-Schiedat A. Cochlear implantation improves hearing and vertigo in patients after removal of vestibular schwannoma. Int Tinnitus J. 2017; 21(1): 2-6