The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 20, Issue 2 / December 2016
Research Paper Pages:76-82
Relationship between Subjective Tinnitus Perception and Psychiatric Discomfort
Authors: Anna Rita Fetoni, Daniela Lucidi, Eugenio De Corso, Antonella Fiorita, Guido Conti, Gaetano Paludetti
PDF
Abstract
Introduction: tinnitus patients have higher risk of developing anxiety-depressive disorders and decreased quality of life. The reasons why selected patients are able to cope with chronic tinnitus, whereas it represents a disabling symptom for others remain under discussion.
Objectives: the objective of the study was to determine the tinnitus-related degree of distress along with the prevalence of anxiety-depression disorders in a sample of eighty patients referring for chronic tinnitus at the Department of Otolaryngology of Catholic University of Rome from March to September 2015.
Materials and Methods: we administered to all patients the Italian versions of Tinnitus Handicap Inventory (THI) and Hospital Anxiety and Depression Scale (HADS). Furthermore we investigated the correlation between patient’s discomfort, severity of hearing loss and age.
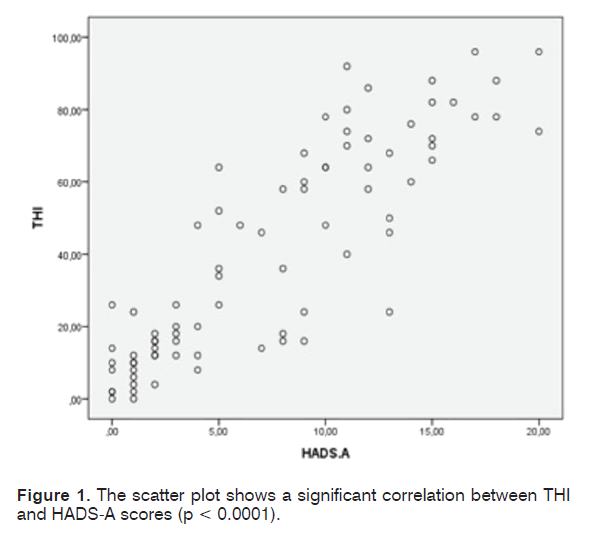
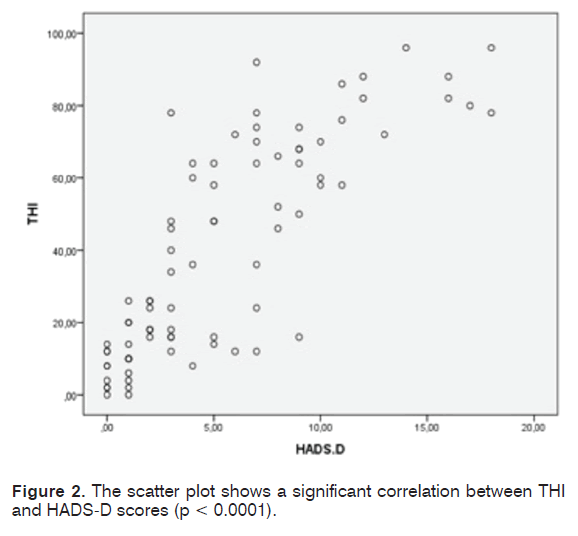
Results: average THI score was 40.85, meaning “moderate” degree of discomfort; 57.5% of the patients showed HADS scores consistent with high risk of psychiatric comorbidities. A significant linear correlation between THI and HADS scores was demonstrated.
Conclusion: we suggest that patients with severe tinnitus-related distress are routinely invited to accomplish psychometric questionnaires, to assess the possibility of a neuropsychiatric evaluation and/or specific pharmacological planning. At this purpose we recommend the administration of HADS, as a reliable and quick instrument.
Keywords: tinnitus, psychometrics, hearing loss, anxiety, depression.
Introduction
Patients suffering from tinnitus have higher risk of developing selected diseases, such as insomnia, anxiety, depression and show a decreased overall quality of life, compared to the general population [1]. In the past decades advancements in neuroscience have made significant steps forward in the understanding of the tinnitus pathophysiological mechanisms. Neuroimaging studies (MRI, fMRI, PET e SPECT) revealed the involvement, in tinnitus, of anatomical structures not classically related with central auditory pathways, such as the parahippocampal area, anterior cingulate cortex, amygdala, insula and frontal lobe [2]. The involvement of these areas, also claimed in the pathogenesis of psychiatric disorders and insomnia, suggests that the relationship between emotional disorders and tinnitus is not random. Association of both disorders would be explained by the arrangement of stable neuronal connections involving the mentioned structures. This neurobiological substratum has a strong clinical implication, since the association between psychiatric disorders (mostly depression and anxiety, but also schizophrenia, obsessive-compulsive syndrome, eating disorders, sleep disorders) and tinnitus ranges between 15 and 75%. It is demonstrated that the degree of tinnitus-related tolerance cannot be explained only by the psychoacoustic measures of tinnitus (i.e. frequency, loudness), duration and/or by the associated hearing impairment. It rather seems that inter-individual differences in subjective perception correlate with the presence of psychiatric comorbidities [4]. Large epidemiological studies demonstrated that 15%- 20% of the adult populations experience some form of tinnitus and one out of five affected patients claims to be emotionally affected [5]. The reasons why some patients are able to live together with tinnitus, whereas it represents a highly disabling symptom for others, remain controversial and still under discussion. Personality factors and subjective ability to cope with stress factors, also known as “hardiness” or “resilience” [6], seem involved in the tinnitus tolerance. The first objective of our study was to determine the tinnitus-related degree of distress along with the prevalence of anxiety-depression disorders in a sample of patients. At this purpose we used Tinnitus Handicap Inventory (THI), the most common and reliable self-administered test for determination of subjective perception suffered by the tinnitus patient. The Italian version of the Hospital Anxiety and Depression Scale (HADS) was administered to evaluate the presence of anxiety and depression. Furthermore we investigated the correlation among patient’s discomfort, severity of hearing loss and age of the subjects.
Materials and Methods
Patients admitted for tinnitus, with or without hearing impairment, at the Department of Otolaryngology of Catholic University of Rome, from March to September 2015, were recruited for the study. Before enrolment all patients received adequate and comprehensible information about the tests administered and gave their written consent to the execution of the tests, according to the Ethical Committee recommendation, in accordance with the ethical standards of the Declaration of Helsinki. Inclusion criteria were: adult patients (age > 35 years), history of tinnitus longer than 3 months, ability to read, understand and answer to the assigned questionnaires. Both patients with and without diagnosis of sensorineural hearing loss at standard tonal audiometry were eligible for the study. All patients underwent audiological evaluation, performed by the same team of audiologists and technicians, including standard pure-tone audiometry, administered under standard conditions, for testing conventional frequency range (0,25 to 8 kHz), using Amplaid 319 audiometer (Amplaid Inc., Milan, Italy) in a double-walled, soundproof room.Tympanometry, acoustic reflex measurement (Grason Stadler Tympstar, Minnesota, USA) and otoscopy were performed in all patients in order to determine the integrity of the conductive mechanism at the time of testing. In selected patients objective techniques such as auditory brainstem responses (ABRs) and otoacoustic emissions (OAEs) (GN Otometrics, Copenhagen, Denmark) or administration of speech audiometry were required in order to better investigate the cause of hearing impairment. Pure-tone average (PTA) values were calculated as the mean of 0.25, 0.5, 1, 2, and 4-kHz thresholds. A validated Italian version of the Tinnitus Handicap Inventory (THI) (Table 1) [7] was administered to determine the subjective perception of tinnitus. This questionnaire consists of 25 questions divided into three subgroups (functional, emotional and catastrophic). Eleven items are included in the functional scale, 9 in the emotional scale and 5 in the catastrophic scale. For each item the patient can assign a value of 0, 2 or 4 points, depending on whether or not he fits himself in the described setting. The final score is used to assign the subject to one of the 5 categories characterized by rising level of distress. The prevalence of anxietydepressive disorder among recruited patients was assessed by the validated Italian version of the Hospital Anxiety and Depression Scale (HADS) (Table 2) [7] a 14 item self-assessment questionnaire allowing measurement of the levels of anxiety and depression experienced by patients referring to non-psychiatric hospital wards. The HADS is divided into two subgroups: the HADS-D for depression and HADS-A for anxiety, each consisting of seven questions. Each item on the questionnaire is scored from 0 to 3 (total final score between 0 and 21 for either anxiety or depression). In both sub-scales the total score of 8 out of 21 indicates the cut-off point for anxiety or depression. Statistical analysis of the collected data was performed using the SPSS 22.0 software (SPSS Inc., Chicago, IL, USA). The bivariate Pearson correlation test was used to determine the degree of correlation between the examined variables, the results were considered significant for p values < 0.05.
| Tinnitus Handicap Inventory (THI) | 4 | 2 | 0 |
|---|---|---|---|
| 1. Because of your tinnitus is it difficult for you to concentrate? | Yes | Sometimes | No |
| 2. Does the loudness of your tinnitus make it difficult for you to hear people? | Yes | Sometimes | No |
| 3. Does your tinnitus make you angry? | Yes | Sometimes | No |
| 4. Does your tinnitus make you confused? | Yes | Sometimes | No |
| 5. Because of your tinnitus are you desperate? | Yes | Sometimes | No |
| 6. Do you complain a great deal about your tinnitus? | Yes | Sometimes | No |
| 7. Because of your tinnitus do you have trouble falling asleep at night? | Yes | Sometimes | No |
| 8. Do you feel as though you cannot escape from your tinnitus? | Yes | Sometimes | No |
| 9. Does your tinnitus interfere with your ability to enjoy social activities (such as going out to dinner, to the cinema)? | Yes | Sometimes | No |
| 10. Because of your tinnitus do you feel frustrated? | Yes | Sometimes | No |
| 11. Because of your tinnitus do you feel that you have a terrible disease? | Yes | Sometimes | No |
| 12. Does your tinnitus make it difficult to enjoy life? | Yes | Sometimes | No |
| 13. Does your tinnitus interfere with your job or household responsibilities? | Yes | Sometimes | No |
| 14. Because of your tinnitus do you find that you are often irritable? | Yes | Sometimes | No |
| 15. Because of your tinnitus is it difficult for you to read? | Yes | Sometimes | No |
| 16. Does your tinnitus make you upset? | Yes | Sometimes | No |
| 17. Do you feel that your tinnitus has placed stress on your relationships with members of your family and friends? | Yes | Sometimes | No |
| 18. Do you find it difficult to focus your attention away from your tinnitus and on to other things? | Yes | Sometimes | No |
| 19. Do you feel that you have no control over your tinnitus? | Yes | Sometimes | No |
| 20. Because of your tinnitus do you often feel tired? | Yes | Sometimes | No |
| 21. Because of your tinnitus do you feel depressed? | Yes | Sometimes | No |
| 22. Do you feel you can no longer cope with your tinnitus? | Yes | Sometimes | No |
| 23. Does your tinnitus get worse when you are under stress? | Yes | Sometimes | No |
| 24. Does your tinnitus make you feel insecure? | Yes | Sometimes | No |
Table 1. Tinnitus Handicap Inventory (THI); in our study a validated Italian translated version was administered[14].
| 1 I feel tense or "wound up": | A |
|---|---|
| A Most of the time | 3 |
| B A lot of the time | 2 |
| C Time to time, occasionally | 1 |
| D Not at all | 0 |
| 2 I still enjoy the things I used to enjoy: | D |
| A Definitely as much | 0 |
| B Not quite so much | 1 |
| C Only a little | 2 |
| D Not at all | 3 |
| 3 I get a sort of frightened feeling like something awful is about to happen: | A |
| A Very definitely and quite badly | 3 |
| B Yes but not too badly | 2 |
| C A little but it doesn't worry me | 1 |
| D Not at all | 0 |
| 4 I can laugh and see the funny side of things: | D |
| A As much as I always could | 0 |
| B Not quite so much now | 1 |
| C Definitely not so much now | 2 |
| D Not at all | 3 |
| 5 Worrying thoughts go through your mind: | A |
| A A great deal of the time | 3 |
| B A lot of the time | 2 |
| C From time to time but not too often | 1 |
| D Only occasionally | 0 |
| 6 I feel cheerful: | D |
| A Not at all | 3 |
| B Not often | 2 |
| C Sometimes | 1 |
| D Most of the time | 0 |
| 7 I can seat at ease and feel relaxed: | A |
| A Definitely | 0 |
| B Usually | 1 |
| C Not often | 2 |
| D Not at all | 3 |
| 8 I feel as if I am slowed down: | D |
| A Nearly all the time | 3 |
| B Very often | 2 |
| C Sometimes | 1 |
| D Not at all | 0 |
| 9 I get a sort of frightened feeling like "butterflies" in the stomach: | D |
| A Not at all | 0 |
| B Occasionally | 1 |
| C Quite often | 2 |
| D Very often | 3 |
| 10 I have lost interest in my appearance: | A |
| A Definitely | 0 |
| B I don't take as much care as I should | 1 |
| C I may not take quite as much care | 2 |
| D I take just as much care as ever | 3 |
| 11 I feel restless as if I have to be on the move: | A |
| A Very much indeed | 3 |
| B Quite a lot | 2 |
| C Not very much | 1 |
| D Not at all | 0 |
| 12 I look forward with enjoyment to things: | D |
| A As much as I ever did | 0 |
| B Rather less than I used to | 1 |
| C Definitely less than I used to | 2 |
| D Hardly at all | 3 |
| 13 I get sudden feelings of panic: | A |
| A Very often indeed | 3 |
| B Quite often | 2 |
| C Not very often | 1 |
| D Not at all | 0 |
| 14 I can enjoy a good book or radio or TV programme: | D |
| A Often | 0 |
| B Sometimes | 1 |
| C Not often | 2 |
| D Very seldom | 3 |
Table 2. Hospital Anxiety and Depression Scale (HADS); in our study a validated Italian translated version was administered [14].
Results
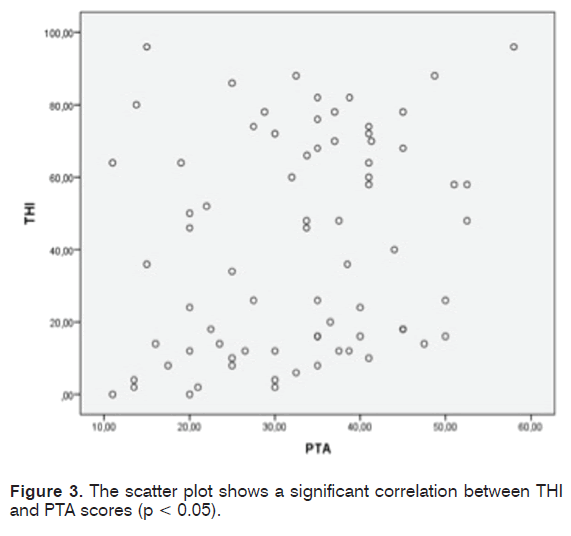
We recruited 80 patients (male-to-female ratio = 0.9); mean age was 68.2 years (SD = 12.9; range = 36-89 years). Mean duration of tinnitus was six years and nine months (SD = 6.1) in the sample of patients examined. The mean value of PTA of both ears was 33.01 dB HL (SD = 12.3; range = 11-58 dB HL). The majority of the examined audiograms showed a bilateral, symmetric, high frequency (i.e. 4 to 8 kHz) hearing loss. Only in 16 patients (20% of the cases) a normal hearing threshold was detected. Average score obtained by THI was 40.85 (SD = 29.85), which stands for “moderate” degree of discomfort. Tinnitus-induced discomfort, in particular, was reputed “slight” by 32,5% of the patients (26/80), “mild” by 15% of the patients (12/80), “moderate” by 12% of the patients (10/80), “severe” by 25% of the patients (20/80), “catastrophic” by 15% of the patients (12/80). Administration of HADS questionnaire to the same sample of patients revealed that 36 patients (45%) (20 women; 16 men) suffer from anxiety symptoms, 21 patients (26.25%) (12 women; 9 men) suffer from depressive symptoms; anxiety and depression were present in combination in 18 patients (22.5%). Seven patients were characterized by a borderline score (4 for the HADS-A and 3 for the HADS-D). Patients not showing any sign of the two disorders were 34 (42.5%). A statistically significant correlation between both the THI and the HADS-A scores (r = 0.87, p<0.0001) (Figure 1) and between the THI and the HADS-D scores (r = 0.813, p < 0.0001) (Figure 2) was demonstrated by the Pearson’s correlation test. Patients were divided into six groups according to age (Table 3). A significant correlation was not established between age and THI score (r = 0.011, p = 0.93). The patients were divided in 3 distinct groups according to the PTA values (Table 4). The Pearson test showed the existence of a not elevated, but still significant correlation (r = 0.24; p = 0.0368) between the hearing loss severity and the THI score (Figure 3). No correlation was determined between duration of tinnitus and THI score (r = 0.003; p = 0.795).
| Age x s n |
|---|
| <40 66 35 3 |
| 40-49 32 39.4 7 |
| 50-59 41.1 31.1 14 |
| 60-69 40 31.5 11 |
| 70-79 37.3 28.6 29 |
| 80-89 48.3 27.2 16 |
Table 3. Age groups; x = THI average scores; s = standard deviation; n = number of patients.
| PTA(dB) x s n |
|---|
| <20 35,5 31,55 16 |
| 21-40 38,6 29,3 41 |
| 41-70 51,7 26,5 23 |
Table 4. PTA groups; x = THI average scores; s = standard deviation; n = number of patients.
Discussion
We determined the tinnitus-related degree of distress and the prevalence of anxiety-depression disorders in patients affected by tinnitus, by administrating Italian versions of Tinnitus Handicap Inventory (THI) and Hospital Anxiety and Depression Scale (HADS). In our series a high prevalence (about 60%) of psychological comorbidities among tinnitus patients was found. The prevalence of patients with anxiety was higher, compared with depressive one (45% vs. 26.25% respectively), according to previous reports [8-9]. THI scores show a strong correlation with both values of the subgroups HADS-A and HADS-D. Our findings demonstrate that severity of subjective tinnitus discomfort is strongly related to the psychological distress measured by HADS. Our results prove that the routine administration of HADS questionnaire, specifically addressed to non-psychiatric patients, is useful in subjects with high risk for developing anxious-depressive symptoms. Accordingly with recent literature, tinnitus patients do not usually meet diagnostic criteria for major depressive disorders but often shows mild psychiatric symptoms, leading to impaired quality of life [4-10]. HADS is a highly sensitive questionnaire, describing the salient features of psychiatric spectrum. Its administration may be helpful in improving audiological counselling and addressing of patients to a specific neuropsychiatric evaluation or cognitive-behavioural therapy. In clinical studies8,9 outcomes significantly differ in terms of both overall prevalence of psychiatric disorder and specific symptoms involved in tinnitus patients. This is probably due to differences in methodological issues (general population studies versus targeted high risk groups of patients; primary care versus tertiary referral hospital), employment of different questionnaires (THI, HADS, VAS) or diagnostic criteria. HADS represents an internationally validated, sensitive tool for detection of somatic and psychiatric symptoms in primary care patients [11]. It is designed according to the actual conditions of the patient, with a relatively short number of items, thus preventing the patient from losing concentration or answer superficially. For these reasons we preferred the use of HADS, rather than other psychometric scales like BADI (Beck Anxiety and Depression Inventory), employed in analogous studies and first used as a comparison for the statistical validation of THI [8,9], consisting of a total of 42 items.
Large epidemiological investigations suggest that a percentage ranging between 10% and 20% of the general population suffers from tinnitus, however only few patients are affected by a marked discomfort leading to a decreased quality of life [12]. The causal relationship between perceived tinnitus severity and psychological/psychiatric impairment is still controversial. The first hypothesis is that the tinnitus may determine the psychiatric condition; on the contrary a pre-existing compensated disorder may be unmasked because of tinnitus. In addition a well-tolerated tinnitus may reappear because of the onset of psychosis [3]. Also, sleep disorders and insomnia, frequently induced by chronic tinnitus, are associated with enhanced depression, anxiety, and somatic symptom severity.
Rauschecker and colleagues [13] focused on the role of limbiccorticostriatal network in subjective perception of tinnitus. It has been demonstrated that, in physiological conditions, the limbic network, including the parahippocampal area, anterior cingulate cortex, amygdala, insula and frontal lobe constitutes a filter for sensory information reaching the level of consciousness. Its action seems to prevent the tinnitus signal from reaching the auditory cortex. Consequently, if the gating circuit involving the amygdala and the subcallosus area is damaged, the subsequent inhibition of thalamic activation can be lost, and the signal is forwarded to the cortex where it is perceived as tinnitus [14]. It has been suggested that, in the long term, this maladaptive reorganization of the auditory cortex may lead to the maintenance of chronic tinnitus in absence of peripheral stimuli and the amplification of its abnormal emotional perception [14]. Our findings suggest that, in patients undergoing severe discomfort related to tinnitus, early and sensitive detection of anxious-depressive symptoms may be achieved, by using the HADS questionnaire. This clinical issue is helpful in redirecting therapeutic strategies, especially considering the lack of an ultimate, well-tolerated, unanimous drug therapy for tinnitus. No recommendation exists in fact on routine use of medication by the US FDA for treatment of tinnitus. However, this statement does not apply to patients with concurrent anxiety or depression disorders. Among the several drugs tested in patients with tinnitus, tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs) and benzodiazepines are included. Although they do not seem to directly reduce the perception of tinnitus, their use could be recommended in those patients affected by anxious-depressive symptoms, regardless of the causal relationship with tinnitus, with the purpose of improving overall quality of life, by indirectly relieving the tinnitus-related distress. We investigated the relationship among hearing impairment, age and tinnitus. The severity of hearing loss appears to have a slight correlation with the THI score, according with Ratnayake [15]. However several authors [10-17] did not confirm this relationship. This result might be influenced by many confounding factors such as age, duration of tinnitus, communication skills and other medical conditions. Some authors suggest that patients with normal hearing may perceive their tinnitus as more annoying because their attention is focused on tinnitus, as a more intrusive symptom, compared with patients with impaired hearing [18]. On the contrary other authors [15,19] suggested that patients with both hearing loss and tinnitus suffer a cumulative annoying effect, justifying higher subjective distress.
Relationship between degree of perceived discomfort and age is still controversial: some authors20 observed that tinnitus causes a deeper discomfort in the elderly, compared to younger people. That could be justified, according to those papers, by changes in plasticity and adaptive mechanisms induced by aging and exogenous factors including noise exposure20. In our case series, however, no significant correlation was demonstrated between age and THI score. It has been suggested that tinnitus, unlike hearing loss, constitutes a weakening symptom in both old and young subjects and that subjective resilience against tinnitus may depend primarily on the individual adaptability [17]. On the contrary, relationship between hearing loss and resulting degree of stress seems far more established in the literature. Auditory deprivation in fact is known to trigger a vicious circle in older people, involving social isolation, quality of life deterioration, depression and cognitive impairment. Our findings confirm that patients with chronic tinnitus show a significantly higher prevalence of anxietydepressive profile, compared to the general population. Therefore we suggest that patients with THI score > 38 are routinely invited to accomplish specific psychometric questionnaires for the presence of psychiatric symptoms, such as HADS. The subjective discomfort triggered by perception of tinnitus represents the main criteria for planning a neuropsychiatric evaluation, in order to establish a pharmacological or cognitive-behavioural therapy. The presence of associated negative symptoms, such as anxiety, depression and insomnia, are crucial for the deterioration of the quality of life.
References
- Cho CG, Chi JH, Song JJ, Lee EK, Kim BH. Evaluation of anxiety and depressive levels in tinnitus patients. Korean J Audiol. 2013;17:83-9.
- Joos K, Vanneste S, De Ridder D. Disentangling depression and distress networks in the tinnitus brain. PLoS One. 2012;7(7):e40544.
- Langguth B, Landgrebe M, Kleinjung T, Sand GP, Hajak G. Tinnitus and depression. World J Biol Psychiatry. 2011;127:489-500.
- Pattyn T, Van Den Eede F, Vanneste S, Cassiers L, Veltman DJ, Van De Heyning P, et al. Tinnitus and anxiety disorders: A review. Hear Res. 2016;333:255-65.
- Eggermont JJ, Roberts LE. The neuroscience of tinnitus. Trends Neurosci. 2004;27:676-82.
- Wallhäusser FE, Mahlke C, Oliva R, Braun S, Wenz G, Langner G. Expression of c-fos in auditory and non-auditory brain regions of the gerbil after manipulations that induce tinnitus. Exp Brain Res. 2003;153:649-54.
- Monzani D, Genovese E, Marrara A, Gherpelli C, Pingani L, Forghieri M, et al. Validity of the Italian adaptation of the Tinnitus Handicap Inventory; focus on quality of life and psychological distress in tinnitus-sufferers. Acta Otorhinolaryngol Italy. 2008;28:126-34.
- Granjeiro RC, Kehrle HM, de Oliveira TS, Sampaio AL, de Oliveira CA. Is the degree of discomfort caused by tinnitus in normal-hearing individuals correlated with psychiatric disorders? Otolaryngol Head Neck Surg. 2013;148:658-63.
- Belli S, Belli H, Bahcebasi T, Ozcetin A, Alpay E, Ertem U. Assessment of psychopathological aspects and psychiatric comorbidities in patients affected by tinnitus. Eur Arch Otorhinolaryngol. 2008;265:279-85.
- Cieśla K, Lewandowska M, Skarżyński H. Health-related quality of life and mental distress in patients with partial deafness: preliminary findings. Eur Arch Otorhinolaryngol. 2016;273:767-76.
- Iani L, Lauriola M, Costantini M. A confirmatory bifactor analysis of the Hospital Anxiety and Depression Scale in an Italian community sample. Health Qual Life Outcomes. 2014;5:12-84.
- Baguley D, McFerran D, Hall D. Tinnitus. Lancet. 2013;382:1600-7.
- Rauschecker JP, Leaver AM, Muhlau M. Tuning out the noise: limbic-auditory interactions in Tinnitus. Neuron. 2010;66:819-26.
- Leaver AM, Renier L, Chevillet MA, Morgan S, Kim HJ, Rauschecker JP. Dysregulation of limbic and auditory networks in tinnitus. Neuron. 2011;69:33-43.
- Ratnayake SA, Jayarajan V, Bartlett J. Could an underlying hearing loss be a significant factor in the handicap caused by tinnitus? Noise Health. 2009;11:156-60.
- Savastano M. Tinnitus with or without hearing loss: are its characteristics different? Eur Arch Otorhinolaryngol. 2008;265:1295-300.
- Pinto PC, Sanchez TG, Tomita S. The impact of gender, age and hearing loss on tinnitus severity. Braz J Otorhinolaryngol. 2010;76:18-24.
- Pajor AM, Ormezowska EA, Jozefowicz-Korczynska M. The impact of co-morbid factors on the psychological outcome of tinnitus patients. Eur Arch Otorhinolaryngol. 2013;270:881-8.
- Zarenoe R, Ledin T. Quality of life in patients with tinnitus and sensorineural hearing loss. B-ENT. 2014;10:41-51.
- Schlee W, Kleinjung T, Hiller W, Goebel G, Kolassa IT, Langguth B. Does tinnitus distress depend on age of onset? PLoS One. 2011;6:e27379.
References
Department Head and Neck Surgery - Institute of Otorhinolaryngology, Catholic University of Sacred Heart. Rome, Italy. Email: afetoni@rm.unicatt.it, dani.lucidi@gmail.com, eugenio.decorso@gmail.com, antofiorita@libero.it, guido.conti@rm.unicatt.it, gaetano.paludetti@rm.unicatt.it
Institution: Department Head and Neck Surgery - Institute of Otorhinolaryngology, Catholic University of Sacred Heart, Rome, Italy
Send correspondence to:
Daniela Lucidi
Largo A. Gemelli n.1, 00168, Rome, Italy. +39 630154439. E-mail: dani.lucidi@gmail.com
Paper submitted to the ITJ-EM (Editorial Manager System) on July 05, 2016; and accepted on October 21, 2016.
Citation: Fetoni AR, Lucidi D, De Corso E, Fiorita A, Conti G, Paludetti G. Relationship between Subjective Tinnitus Perception and Psychiatric Discomfort. Int Tinnitus J. 2016; 20(2): 76-82