The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 22, Issue 2 / December 2018
Original Paper Pages:97-102
10.5935/0946-5448.20180017
Anterior Cervical Osteophytes and Sympathetic Hyperactivity in Patients with Tinnitus: Size Matters
Authors: Henk M. Koning, Mark V. Koning, Nick J. Koning, Bas C. ter Meulen
PDF
Abstract
Context: Pathological changes secondary to degeneration of the cervical intervertebral disc may cause irritation of sympathetic nerve fibers, leading to sympathetic symptoms and tinnitus.
Objectives: The aim of this study was to relate the effect of percutaneous radiofrequency treatment of superior cervical sympathetic ganglion in patients with tinnitus to cervical pathology.
Method: A retrospective study of 74 consecutive patients who underwent treatment of the superior cervical sympathetic ganglion for tinnitus that persisted for 1 month or longer from October 2016 to January 2018. The work-up of a patient with tinnitus consisted of a standardized clinical history, a bilateral audiogram and a cervical spine radiograph.
Results: All patients had a test blockade of superior cervical sympathetic ganglion first, and 54% of these patients (n=40) responded with a reduction of their tinnitus. These patients underwent a radiofrequency lesion and 53% (n=21) responded with a reduction of their tinnitus at 7 weeks following treatment. The size of anterior osteophyte at the fifth cervical vertebrae was related to a positive response at 7 weeks following this treatment. Patients with tinnitus and an anterior osteophyte at vertebrae C5 more than 17% of the width of those vertebrae had a success rate of 52% following treatment of the superior cervical sympathetic ganglion, compared to 13%, when the anterior osteophyte at C5 was 17% or less.
Conclusions: The size of anterior cervical osteophytes is associated with a higher success rate of radiofrequency lesions of the superior sympathetic ganglion for tinnitus. The current results imply a role for cervical sympathetic nervous system irritation in the development of tinnitus in a subgroup of patients.
Keywords: tinnitus, superior cervical ganglion, radiofrequency ablation, sympathetic ganglia, sympathetic nervous system
Introduction
Tinnitus is a frequently debilitating symptom of which the underlying pathophysiology is incompletely understood [1]. Multiple theories have been suggested, one of which includes that tinnitus may be related to a reduced blood circulation to the inner ear [2]. Sympathetic fibers innervating the cochlea play a role in control of cochlear blood flow with direct sympathetic-induced vasoconstriction [3-5]. Blockade of the sympathetic fibers to the cochlea may reduce local vasoconstriction and has been described as therapy for tinnitus in a subgroup of patients [6].
Cochlear sympathetic innervation mainly originates at the superior cervical ganglion or at the stellate ganglion [7]. Pathological changes secondary to degeneration of the cervical intervertebral disc may cause irritation of sympathetic nerve fibers [8]. To our knowledge, the relation between cervical spine pathology and the efficacy of sympathetic therapy has never been assessed. Therefore, the aim of this study was to relate the effect of percutaneous radiofrequency treatment of superior cervical sympathetic ganglion in patients with tinnitus to cervical spine pathology. We hypothesized that the presence of radiographic cervical spine abnormalities was associated with a higher response rate to percutaneous radiofrequency treatment of superior cervical sympathetic ganglion in patients with tinnitus.
Methodology
Subjects
The Medical research Ethics Committees United (Nieuwegein, the Netherlands) approved the present observational study and waived the request for informed consent for the current study. A retrospective chart review was conducted. All patients that were treated with an initial test blockade of the superior cervical sympathetic ganglion to our clinic between October 2016 and January 2018 for tinnitus that persisted for 1 month or longer were included. There were no exclusion criteria. All patients were previously consulted by an otorhinolaryngologist and all patients who suffered with unilateral tinnitus had anatomical pathology ruled out by MRI. The workup of a patient with tinnitus consisted of a standardized clinical history, a bilateral audiogram and a cervical spine radiograph. The standardized clinical history included tinnitus characteristics (left side and/or right side, traumatic cause, duration of complaints and age of onset, and concomitant symptoms (self-reported hearing loss, the presence of dysbalance, dizziness, and cervicalgia).
A standardized bilateral clinical audiogram assessed pure tone thresholds at 125, 250, 500, 1000, 2000, 4000, and 8000 Hz.
The lateral cervical spine radiographs were assessed for:
• The angle between the posterior border of consecutive cervical vertebrae.
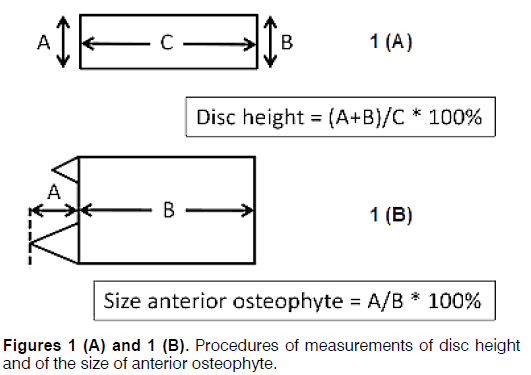
• The intervertebral disc space height of the five cervical levels, as assessed by the Farfan’s measurement (FM): (anterior disc height+posterior disc height)/disc diameter × 100% (Figure 1A) [9].
• The size of the anterior osteophyte relative to the size of the cervical vertebrae, as calculated by dividing the distance of the anterior border of the largest anterior osteophyte to the anterior border of the cervical vertebrae by the width of the cervical vertebrae at the middle × 100% (Figure 1B).
Treatment of the Superior Cervical Sympathetic Ganglion
All injections of the superior cervical sympathetic ganglion were performed by an experienced anesthesiologist (HMK) in a routine manner on an outpatient basis.
The blockade of the superior cervical sympathetic ganglion was carried out with the patient lying supine on an X-ray table. No premedication or sedation was used so that the patients would be able to report the pain sensations during the procedure. Under X-ray guidance, a 23-gauge radiofrequency top-pole needle with an active tip of 5 mm (Top Neuropole needle XE-S, Tokyo, Japan) was inserted for the test blockade and for the radiofrequency lesion. All blocks were performed as previously described [6],[10]. In lateral projection, the entry point of the needle was chosen at the level of the facet joint of the third and fourth cervical vertebrae. The direction of radiographic projection was changed in such a way that the facetal column was projected over the anterolateral aspect of the vertebral bodies. After disinfecting the puncture site with 60% chlorhexidine in alcohol, the needle was introduced parallel to the radiographic projection and was projected as a dot approximately 1 cm anterior to the spine. The radiographic projection was then changed to lateral, and the needle was slowly advanced until the tip was situated at the anterior border of the third cervical vertebra. On the anteroposterior projection, the aim was to project the tip of the needle over the lateral part of the facetal column. When the tip of the needle was in position, 0.3 mL of Iohexol (Omnipaque, Eindhoven, the Netherlands) was injected. On the transverse projection, the aim of the contrast was to lie distinctly anterior to anterior border of the vertebral bodies and in the anteroposterior projection the contrast was aimed to spread in a space overlying the facetal column in a cranial as well as caudal direction. The correct position of the needle was subsequently verified by an electrical stimulus of 50 Hz. Paraesthesia should be obtained at the lateral aspect of the neck with less than 1.0 V, the needle was repositioned if necessary. During the test blockade, bupivacaine 0.25% 1.5 mL (Bupivacaine Aurobindo, Baarn, the Netherlands) was injected. If the patient reported a significant reduction of the tinnitus (i.e., 25% or more), the same procedure was repeated again to produce a radiofrequency lesion of the superior cervical sympathetic ganglion. The superior cervical sympathetic ganglion was then anaesthetized with 2 mL lignocaine 2% (Lidocaïne HCL Braun, Melsungen, Germany) followed by a radiofrequency lesion of 16 V for 60 seconds using the NeuroTherm® TLG-10 radiofrequency lesion generator (Neurotherm Inc., Wilmington, MA, USA). No temperature monitoring or any other testing besides the electrical stimulus of 50 Hz was used. The patients were being observed and monitored in the recovery room for a minimal of 30 minutes and discharged home. All patients were re-evaluated by the interventionist 7 weeks after treatment.
Data assessment
Patient charts were reviewed retrospectively to identify those who underwent a treatment of the superior cervical sympathetic ganglion for tinnitus. Data recorded from these patients were patient characteristics (age, sex), tinnitus characteristics (left side and/or right side, traumatic, duration of complaints, and age of onset), comorbidity (self-reported hearing loss, the presence of misbalance, dizziness, and cervicalgia), and self-reported benefit from treatment after 7 weeks. The results of the audiogram were obtained for the ear in which the tinnitus predominated. If the tinnitus was perceived as equal between both sides the average of the results of the audiogram of both sides were computed and used. The above mentioned measurements of the cervical spine radiograph were obtained.
Statistical methods
Statistical analysis was performed with Minitab 16 (Minitab Inc., State College, PA, USA). A Chi-square test was used for dichotomous variables, and Student’s t-test was used for continuous variables. Discriminant analysis for division in two groups was used to evaluate the correlation of the most significant variable of the measurements of the cervical spine radiograph with the self-reported benefit from treatment of the superior cervical sympathetic ganglion in patients with tinnitus. Data are presented as Mean (Standard Error of the Mean) unless otherwise specified. A value of P<0.05 was considered statistically significant.
Results
From October 2016 to January 2018, 74 patients underwent treatment of the superior cervical sympathetic ganglion to treat their tinnitus. Forty patients (54%) responded with a reduction of their tinnitus (i.e. 25% or more) to the test blockade. These responders underwent a radiofrequency lesion and 21 patients (53%) responded with a reduction of their tinnitus at 7 weeks following treatment.
Patients with a positive effect of a radiofrequency lesion of the superior cervical sympathetic ganglion on the tinnitus at 7 weeks were compared with the nonresponders (Table 1). The presence of vertigo, cervical pain, and the severity of hearing loss at 125, 250, 500, and 1000 was increased in the responders as compared to non-responders to treatment. The size of anterior osteophyte at the vertebrae C5 was greater in patients with to a positive response at 7 weeks following superior cervical sympathetic ganglion treatment compared to non-responding patients.
| Condition | Responders (n=21) | Non-responders (n=53) | P-value | |||
|---|---|---|---|---|---|---|
| Prevalence | Mean SEM | Prevalence | Mean SEM | |||
| Vertigo | 57% | - | 30% | - | 0.031 | |
| Self-perceived hearing loss | 81% | - | 68% | - | 0.262 | |
| Cervical pain | 90% | - | 53% | - | 0.003 | |
| Hearing loss (dB) at: | ||||||
| - 125 Hz | - | 41.6 8.4 | - | 18.1 3.7 | 0.030 | |
| - 250 Hz | - | 32.9 6.3 | - | 18.2 2.4 | 0.041 | |
| - 500 Hz | - | 33.1 5.9 | - | 18.2 2.2 | 0.027 | |
| - 1 KHz | - | 35.0 5.7 | - | 19.3 2.4 | 0.019 | |
| - 2 KHz | - | 32.5 5.2 | - | 23.4 2.5 | 0.122 | |
| - 4 KHz | - | 47.7 5.9 | - | 39.1 3.1 | 0.210 | |
| - 6 KHz | - | 67.6 7.0 | - | 51.8 4.0 | 0.069 | |
| - 8 KHz | - | 55.5 6.7 | - | 49.8 3.4 | 0.454 | |
| Angle between vertebrae (degrees): | ||||||
| -C2-C3 | - | 4.3 0.8 | - | 3.1 0.7 | 0.265 | |
| -C3-C4 | - | 2.0 0.9 | - | 1.5 0.8 | 0.676 | |
| -C4-C5 | - | 0.9 1.0 | - | 1.80.6 | 0.475 | |
| -C5-C6 | - | 0.5 1.0 | - | 1.20.7 | 0.590 | |
| -C6-C7 | - | 4.5 1.5 | - | 3.1 0.7 | 0.419 | |
| Farfan’s measurement of disc space height (%): | ||||||
| -C2-C3 | - | 38.4 1.5 | - | 40.6 1.0 | 0.237 | |
| -C3-C4 | - | 34.0 1.7 | - | 37.4 1.4 | 0.126 | |
| -C4-C5 | - | 35.9 1.4 | - | 36.0 1.4 | 0.962 | |
| -C5-C6 | - | 26.7 1.8 | - | 28.7 1.4 | 0.404 | |
| -C6-C7 | - | 26.2 2.2 | - | 27.6 1.6 | 0.609 | |
| Size of anterior osteophyte (%) at: | ||||||
| -C3 | - | 5.3 1.3 | - | 5.7 0.9 | 0.838 | |
| -C4 | - | 8.61.3 | - | 10.5 1.2 | 0.269 | |
| -C5 | - | 19.8 1.3 | - | 15.3 1.1 | 0.009 | |
| -C6 | - | 12.8 1.5 | - | 12.6 1.2 | 0.930 | |
| dB: decibel, Hz: Hertz, KHz: Kilohertz, SEM: Standard error of the mean. | ||||||
Table 1. Sociodemographic features of the patients (N=132).
Discriminant analysis of all the patients showed an anterior osteophyte at vertebrae C5 of more than 17% of the width of that vertebrae was associated with a higher success rate following treatment of the superior cervical sympathetic ganglion (Proportion Correct=0,730). Patients with an anterior osteophyte at vertebrae C5 of more than 17% of the width of the vertebrae were compared to the other patients in Table 2. Patients with this anterior osteophyte at vertebrae C5 were characterized by disc degeneration at C5-C6 and C6-C7 and larger anterior osteophyte at the vertebrae C6. In these patients, 52% of them had a reduction of their tinnitus at 7 weeks following treatment of the superior cervical sympathetic ganglion. If there was a positive test-blockade before the radiofrequency lesion the success-rate of this therapy increased to 65%.
| Condition | Anterior osteophyte at C5 larger than 17% | Anterior osteophyte at C5 of 17% or less | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Prevalence | Mean SEM | Prevalence | Mean SEM | ||||||
| Number of patients (%) | 29 (39%) | - | 45 (61%) | - | |||||
| Vertigo | 48% | - | 31% | - | 0.137 | ||||
| Self-perceived hearing loss | 76% | - | 69% | - | 0.516 | ||||
| Cervical pain | 79% | - | 53% | - | 0.03 | ||||
| Effect all patients SCGS: | 52% | - | 13% | - | 0 | ||||
| Effect Rf SCGS after positive test: | 65% | - | 35% | - | 0.061 | ||||
| Farfan’s measurement of disc space height (%): | |||||||||
| -C2-C3 | - | 40.0 1.0 | - | 40.4 1.0 | 0.729 | ||||
| -C3-C4 | - | 35.7 1.4 | - | 37.5 1.2 | 0.332 | ||||
| -C4-C5 | - | 35.9 1.3 | - | 35.7 1.2 | 0.913 | ||||
| -C5-C6 | - | 22.8 1.3 | - | 31.3 1.1 | 0 | ||||
| -C6-C7 | - | 23.8 1.4 | - | 29.4 1.4 | 0.005 | ||||
| Size of anterior osteophyte (%) at: | |||||||||
| -C3 | - | 7.0 1.0 | - | 4.9 0.7 | 0.084 | ||||
| -C4 | - | 10.6 0.9 | - | 8.9 1.0 | 0.175 | ||||
| -C5 | - | 23.4 0.7 | - | 11.4 0.6 | 0 | ||||
| -C6 | - | 16.0 1.2 | - | 10.4 0.9 | 0 | ||||
| SEM: Standard error of the mean. Rf: Radiofrequency lesion; SCSG: superior cervical sympathetic ganglion | |||||||||
Table 2. Patient characteristics for patient groups with the presence or absence of an anterior osteophyte at the fifth vertebrae larger than 17% of the width of the fifth vertebrae.
An anterior osteophyte at the fifth cervical vertebrae larger than 17% of the width of the fifth vertebrae lesion has a sensitivity of 65% and a specificity of 58% in predicting the effect of superior cervical sympathetic ganglion treatment in patients with tinnitus. The positive and negative predictive values were 71% and 58% respectively.
No adverse events of the radiofrequency lesion of the superior cervical sympathetic ganglion were reported at 7 weeks of follow-up.
Discussion
The current study shows that the presence of major anterior osteophytes at the cervical vertebral column increases are associated with an improved response to a radiofrequency lesion of the superior cervical sympathetic ganglion in tinnitus patients. This finding supports the theory that the sympathetic nervous system is an important contributor to tinnitus in a subgroup of patients [11].
Tinnitus has previously been associated with cervical pathology [12] and cervical spine abnormalities can manifest itself as hearing loss, vertigo, or tinnitus [12-14]. Especially the upper segments of the cervical spine are considered in the pathogenesis of tinnitus [13]. In the current study the lower cervical segments from C5 to C7 showed the most prominent abnormalities, which are cervical disc degeneration at C5-C6 and C6-C7 together with large anterior osteophytes at the fifth and sixth cervical vertebrae.
Somatosensory modulation of tinnitus originates from the complex somatosensory-auditory interactions arising from the temporomandibular joint, craniocervical junction, cervical vertebrae, and neck and shoulder muscles [15]. Somatic disorders have been shown to play a central role in a large portion of patients with tinnitus and, when correctly identified and treated, can represent a valid therapeutic option. Somatic testing may identify patients who could be treated with somatosensory system-related therapies [16]. Therefore, the aim of this study was to relate the effect of sympathetic therapy in patients with tinnitus to cervical spine pathology.
The current results imply a role of cervical spine pathology and sympathetic nervous system irritation in the pathogenesis of tinnitus in a subgroup of patients. Clinical reports of the relationship between the cervical sympathetic nerves and complaints of tinnitus, dizziness, hearing loss, headache, and neck pain have been called the Barré–Liéou syndrome [6],[17]. The syndrome is believed to be caused by trauma or degeneration of the cervical column with a protrusion of the anterior border of the third and fourth cervical vertebrae or disks irritating the cervical sympathetic nerves, and resulting in local vasoconstriction. The sympathetic nervous system plays a significant role in the control of cochlear microcirculation, and the superior cervical ganglion is probably the main origin of sympathetic fibers which innervate the cochlear vessels [3-5]. Blockade of the sympathetic fibers to the cochlea has previously been reported to reduce the intensity of tinnitus [6]. In the current study we show that, in addition to the previously described middle cerebral vertebrae, the lower cervical vertebral column can also produce symptoms as in the Barré-Liéou syndrome.
In our study, a reduction of tinnitus following a radiofrequency lesion of the superior cervical sympathetic ganglion was seen in 53% of the patients with tinnitus who had a positive test blockade first. This is similar to the numbers that Matoba et al. found in patients with vibration disease [18]. Presence of vertigo, cervical pain, a lowfrequency hearing loss and larger anterior osteophyte at the C5 vertebrae are characteristics that predict a positive effect of RF treatment. Especially the anterior osteophyte is discriminating for a positive result, since patients with the presence of an osteophyte had a success rate of 52% compared to a success rate of 13% for patients without an osteophyte. Using the size of anterior osteophyte at the fifth cervical vertebrae as diagnostic test for performing superior cervical sympathetic ganglion treatment in patients with tinnitus, positive and negative predictive values of 71% and 58% could be obtained, respectively. A positive response to test blockade of the superior cervical sympathetic ganglion will further support the diagnosis and will also increase the success-rate of this treatment.
This study has several limitations. First, the current retrospective study comes with inherent limitations. A prospective follow-up study would be necessary to confirm these results. Second limitation is the number of patients in this study. Even though these numbers are sufficient to demonstrate an effect in this explorative study, re-evaluation of these predictors are necessary in a larger cohort. Although it has been hypothesized that blockade of the superior cervical sympathetic ganglion improves tinnitus symptoms by increasing cochlea blood flow, this has not been investigated in the current study and therefore remains a hypothesis.
Conclusion
The current study shows that large anterior cervical osteophytes are associated with an improved treatment effect of radiofrequency lesions of the superior cervical sympathetic ganglion in patients with tinnitus. In particular, discriminant analysis showed that the presence of an anterior osteophyte at vertebrae C5 of more than 17% of the width of that vertebrae in patients with tinnitus was associated with an improvement with treatment of the superior cervical sympathetic ganglion. In patients with persistent tinnitus, radiographic study of the cervical spine and treatment of the superior cervical sympathetic ganglion may be considered.
References
- Baguley D, McFerran D, Hall D. Tinnitus. Lancet. 2013;382(9904):600-7.
- Nakashima T, Naganawa S, Sone M, Tominaga M, Hayashi H, Yamamoto H, et al. Disorders of cochlear blood flow. Brain Res Rev. 2003;43(1):17-28.
- Laurikainen EA, Kim D, Didier A, Ren T, Miller JM, Quirk WS, et al. Stellate ganglion drives sympathetic regulation of cochlear blood flow. Hear Res. 1993;64(2):199-204.
- Miller JM, Ren TY, Nuttall AL. Studies of inner ear blood flow in animals and human beings. Otolaryngol Head Neck Surg. 1995;112(1):101-13.
- Ren TY, Laurikainen E, Quirk WS, Miller JM, Nuttall AL. Effects of electrical stimulation of the superior cervical ganglion on cochlear blood flow in guinea pig. Acta Otolaryngol. 1993;113(2):146-51.
- Koning HM, Dyrbye BA, van Hemert FJ. Percutaneous radiofrequency lesion of the superior cervical sympathetic ganglion in patients with tinnitus. Pain Practice. 2016;16(8):994-1000.
- Bartolomé MV, Gil-Loyzaga P. Serotonergic innervation of the inner ear: Is it involved in the general physiological control of the auditory receptor? Int Tinnitus J. 2005;11(2):119-25.
- Wang Z, Wang X, Yuan W, Jiang D. Degenerative pathological irritations to cervical PLL may play a role in presenting sympathetic symptoms. Med Hypotheses. 2011;77(5):921-3.
- Frobin W, Brinckmann P, Biggemann M. Objective measurement of the height of lumbar intervertebral disks from lateral roentgen views of the spine. Z Orthop Ihre Grenzgeb. 1997;135(5):394-402.
- Koning HM, Koning AJ, Bruinen TCM, Koster HG. Percutaneous radiofrequency lesion of the superior cervical sympathetic ganglion in non-traumatic neck pain. Pain Clinic. 2000;12(4):271-9.
- van der Loo E, Congedo M, Vanneste S, Van De Heyning P, De Ridder D. Insular lateralization in tinnitus distress. Auton Neurosci. 2011;165(2):191-4.
- Montazem A. Secondary tinnitus as a symptom of instability of the upper cervical spine: Operative management. Int Tinnitus J. 2000;6(2):130-3.
- Kessinger RC, Boneva DV. Vertigo, tinnitus, and hearing loss in the geriatric patient. J Manipulative Physiol Ther. 2000;23(5):352-62.
- Vasaghi-Gharamaleki B, Naser Z. Predicting the risk of hearing impairment following the cervical spine diseases by measuring the cervical range of movements: A pilot Study. Basic Clin Neurosci. 2017;8(5):413-8.
- Ralli M, Greco A, Turchetta R, Altissimi G, de Vincentiis M, Cianfrone G. Somatosensory tinnitus: Current evidence and future perspectives. J Int Med Res. 2017;45(3):933-947.
- Haider HF, Hoare DJ, Costa RFP, Potgieter I, Kikidis D, Lapira A, et al. Pathophysiology, diagnosis and treatment of somatosensory tinnitus: A scoping review. Front Neurosci. 2017;11:207.
- Pearce JMS. Barré-Liéou "syndrome". J Neurol Neurosurg Psychiatry. 2004;75(2):319.
- Matoba T, Noguchi I, Noguchi H, Sakurai T. Stellate ganglion block for the relief of tinnitus in vibration disease. Kurume Med J 1984;31(4):295-300.
References
1Department of Pain therapy, Pain Clinic De Bilt, De Bilt, The Netherlands
2Department of Anesthesiology, Haaglanden Hospital, The Hague, The Netherlands
3Department of Anesthesiology, VU University Medical Center, Amsterdam, The Netherlands
4Department of Neurology, OLVG, Amsterdam, and Zaans Medisch Centrum, Zaandam, The Netherlands
Send correspondence to:
Henk M. Koning Department of Pain therapy, Pain Clinic De Bilt, 3732 AG De Bilt, The Netherlands. E-mail: hmkoning@pijnkliniekdebilt.nl
Paper submitted to the ITJ-EM (Editorial Manager System) on July 03, 2018; and accepted on June 25, 2018.
Citation:Koning HM, Koning MV, Koning NJ, Meulen BCT. Anterior Cervical Osteophytes and Sympathetic Hyperactivity in Patients with Tinnitus: Size Matters. Int Tinnitus J. 2018;22(2):97-102.