The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 26, Issue 1 / June 2022
Research Article Pages:68-74
10.5935/0946-5448.20220010
Association of Tinnitus with Anxiety and Depression among Active-Duty Army Personnel and Veterans at Hospital Angkatan Tentera Tuanku Mizan, Malaysia
Authors: Reuben Thomas, Asma A, Noor Dina H, Loh Sheau Torng, Aniza Ismail, Shalisah Sharip
PDF
Abstract
Objectives: To study the prevalence of tinnitus, its characteristic and its association with anxiety and depression among active-duty army personnel and veterans. This study also wants to determine the correlation of Tinnitus Handicap Inventory (THI) with Hospital Anxiety Depression Scale (HADS) among active-duty army personnel and veterans at Hospital Angkatan Tentera Tuanku Mizan.
Materials and Methods: A cross-sectional study was conducted at the Otorhinolaryngology Head and Neck Surgery Department of Hospital Angkatan Tentera Tuanku Mizan from January 2020 until June 2021, involving active-duty army personnel and veterans with at least 3 years of service. Those patients who fulfilled inclusion and exclusion criteria were recruited. Their feedback was recorded based on Malay version of Tinnitus Handicap Inventory (THI) and Malay version of Hospital Anxiety Depression Scale (HADS)
Results: 106 subjects responded to our questionnaires, (51 active-duty army personnel and 55 veterans) in which 4.7% (n=5) reported to have anxiety and none had depression. Overall mean score for Total THI was 27.66, suggesting that majority of our subjects only felt mild handicap due to their tinnitus. Individual THI subdomain mean scores shows that the functional subdomain (17.79) affects subjects the most as compared to the emotional (5.7) and catastrophic scores (4.21)
Conclusion: Tinnitus can occur in all degrees of hearing loss, and it is associated with poor functional THI scores. Tinnitus is associated with anxiety but not depression among army personnel. These findings suggest that tinnitus should be addressed by healthcare providers in the military in order to maximise function and Quality of Life (QOL) among the nation’s military personnel.
Keywords: Tinnitus, Anxiety, Depression, Veterans, Active-duty army personnel, Hearing loss
Introduction
Tinnitus is a common medical symptom that can be debilitating. It is derived from the Latin verb tinnire (to ring), the term tinnitus describes the conscious perception of an auditory sensation in the absence of a corresponding external stimulus. Tinnitus can be subjective, when the experience is of the individual alone, or, less commonly, objective, when an observer can hear the tinnitus. The sensation is generally of an elementary naturedescriptions of hissing, sizzling, and ringing are common. Tinnitus can sometimes be rhythmical or pulsatile. Pulsatile tinnitus can be synchronous with the heartbeat, in which case a vascular origin is likely, or asynchronous, in which case myoclonus of middle-ear or palatal muscles is probable [1,2]. Tinnitus can be constant or intermittent, and many patients experience more than one sound. It can be localised to one or both ears, and centrally within the head, although some patients describe an external point of origin. The onset of tinnitus can be abrupt, but it is insidious in most cases.
Tinnitus has been further classified according to its initial triggers as primary tinnitus, which is either associated with Sensorineural Hearing Loss (SNHL) or is idiopathic (or unknown cause), and secondary tinnitus, which is related to other causes such as an organic origin3. Large-scale population studies have identified other risk factors such as vascular disease, hypertension, diabetes, autoimmune disorders, head injury, and degenerative neural disorders [4,5]. A fundamental question in tinnitus pathophysiology concerns the neural component that generates tinnitus [6,7] initially postulated that tinnitus could originate in any relevant anatomical structure, from the ear throughout the central auditory pathways. Initial speculations favored a cochlear origin since tinnitus can be perceived in the ears and also due to the fact that there is a strong association between the frequency of psychoacoustic identified tinnitus and the audiometric profile of hearing thresholds [8]. Nowadays, it is well established that many forms of tinnitus reflect a complex interaction between peripheral and central mechanisms within the auditory pathway [9]. Usually two or more triggers (e.g., Noise exposure, hearing loss, emotional distress, and somatosensory factors) are necessary to elicit a noticeable tinnitus [10].
In compensated tinnitus, the patient copes well with the tinnitus and there is little or no psychological distress. In decompensated tinnitus however, the tinnitus perception is considered uncontrollable and interferes with the patient’s QOL, causing emotional and psychological distress [11]. Studies has shown that up to 77% of the tinnitus population may present with psychiatric comorbidities because of tinnitus [12]. Among them, anxious and depressive symptoms seem to be the most common complications with tinnitus [13]. Perception of tinnitus and negative emotions are amplified in a vicious negative feedback loop by the limbic system in the amygdala. When they are present together, there is amplification and impairment of signals, resulting in persistence of both emotional and tinnitus symptoms [14].
Tinnitus affects up to 30% of military veterans, a prevalence rate that is twice that of the nonveteran population [7]. According to the American Tinnitus Association, fifty million Americans suffer with tinnitus and tinnitus is the most prevalent service-connected disability among veterans. Ground infantries with bothersome or distracting tinnitus are more likely to have sleep disorders, which in turn affects their concentration, emotional stability, alertness, and the efficiency of operational missions such as stealth and readiness [15]. Whereas Malaysian army is the land component of the Malaysian Armed Forces. The army contributes to the national defence objectives through the provision of land and special operations capabilities. The army also provides security response to a wide range of incidents, such as bush fires, floods, and major events16. Army personnel in particular are exposed to noise levels and blast environments that can cause tinnitus and can serve as a model population for studying the impact on anxiety and depression.
Materials and Methods
This cross-sectional study was done from January 2020 until June 2021, involving the Otorhinolaryngology Head and Neck Surgery Department of Hospital Angkatan Tentera Tuanku Mizan. Veterans and active-duty army personnel with at least 3 years of service and they have complained of at least 3 months of primary subjective tinnitus were recruited in this study. Patients who are illiterate with secondary objective tinnitus, pre-existing anxiety and depression were excluded. A total of 106 participants fulfilled our inclusion criteria in which constituted of 51 active-duty army personnel and 55 veterans, had their medical records traced and responses to the Malay version of HADS and Malay version of THI were recorded. This study received ethical approval from both the university research ethics committee (UKM PPI/111/8/JEP-2021-386) and by the Hospital Angkatan Tentera Tuanku Mizan research ethic committee (HATTM/EK/18-03).
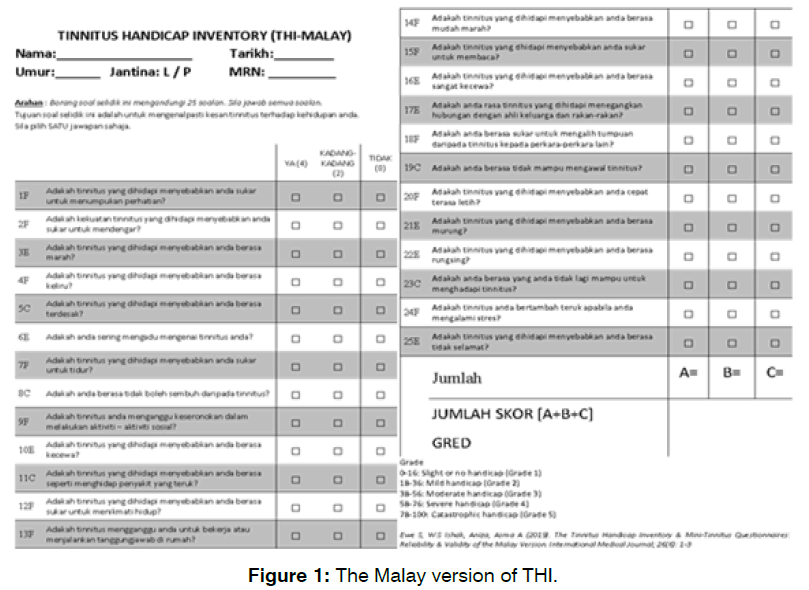
The Malay THI (Figure 1) is a translated and a validated form of the English version of THI that was done by Ewe et al [17]. It is to determine the subjective perception of tinnitus. It consists of 25 questions divided into three subgroups (functional, emotional, and catastrophic). 12 items are included in the functional scale, 8 in the emotional scale and 5 in the catastrophic scale. For each item the patient can assign a value of 0, 2 or 4 points. The final score is used to assign the subject to one of the 5 grades of severity characterized by rising level of handicap
Figure 1: The Malay version of THI.
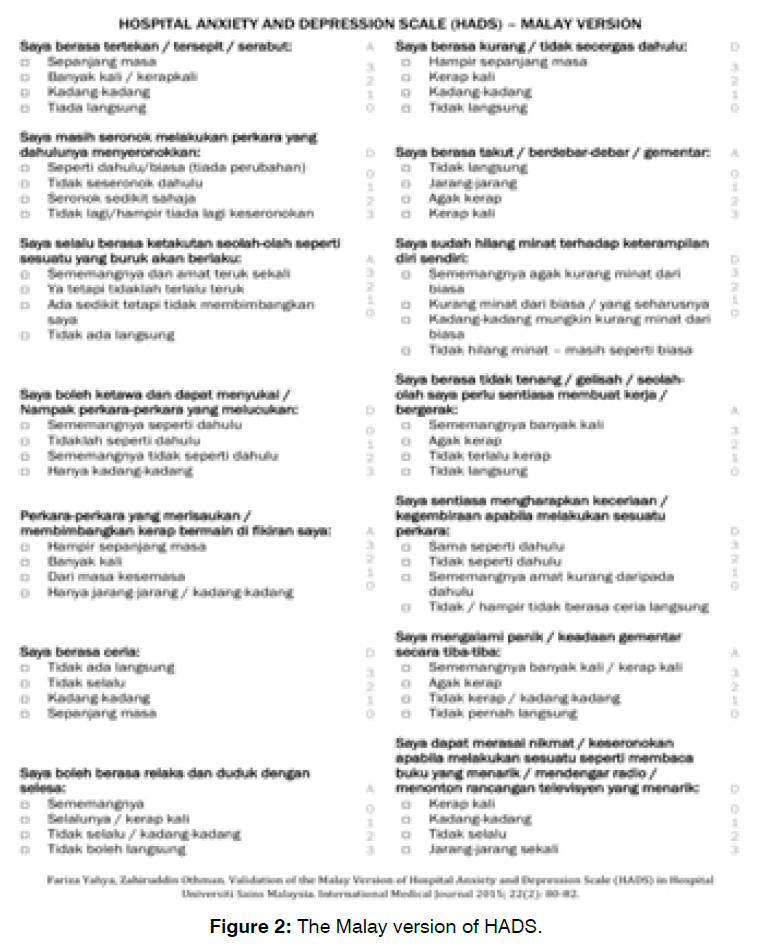
The Malay HADS (Figure 2) is also a translated and validated version of the English HADS that was done by Yahya et al [18]. It is a 14 item self-assessment questionnaire to assess anxiety and depression. HADS is divided into two subgroups: the HADS-D for depression and HADS-A for anxiety, each consisting of 7 questions. Each item on the questionnaire is scored from 0 to 3 (total final score between 0 and 21 for either anxiety or depression). In both sub-scales the total score of 8 indicates the cut-off point for anxiety or depression.
Figure 2: The Malay version of HADS.
Statistical Analysis: Statistical analysis was performed using IBM SPSS 27. Patients’ responses for the HADS and THI questionnaire were taken as the outcome measure. Exploratory data analysis is done to assess for normality using the Shapiro-Wilk test with a statistically significant value of p<.05 signifying that the data is not normally distributed. Spearman’s correlation test was used to test the correlation between THI and HADS.
Results
Out of 938 subjects that were screened throughout our study period, 133 were included in our study in which 106 subjects responded to our questionnaires giving an overall response rate of 79%. The prevalence of tinnitus among the subjects was 11.3% and out of that, 4.7% (n=5) reported to have anxiety and none had depression. Table 1 summarises the demographic data and clinical characteristics of tinnitus perceived by subjects in this study. The mean age of subjects was 58.1 (43-73) years old. Majority of our patients (94.3%) were male and only 6 (5.7%) were female. The Malay race predominates (74.5%) followed by the Chinese (14.2%), Indian (8.5%) and others (2.8%). There was almost equal distribution of subjects, 51 active-duty army personnel (48.1%) and 55 veterans (51.9%). Near two thirds (71.7%) of the subjects had served the army for more than 10 years in service (71.7%) as compared to less than 10 years in service (28.3%). The mean duration of reported tinnitus is 5.3 years. Majority of our subjects reported tinnitus occurs in bilateral ears (52.8%), persistent in character (68.9%), and a low pitch (41.5%) in perception of tinnitus.
| Demographics | n = 106 |
|---|---|
| Age (mean±SD) | 58.17 ±14.9 years |
| Gender | Male 94.3% (n=100) |
| Female 5.7% (n=6) | |
| Race | Malay 74.5% (n=79) |
| Chinese 14.2% (n=15) | |
| Indian 8.5% (n=9) | |
| Others 2.8% (n=3) | |
| Army Personnel | Active-duty personnel 48.1% (n=51) |
| Veterans 51.9% (n=55) | |
| Years in service | Less than 10 years 28.3% (n=30) |
| More than 10 years 71.7% (n=76) | |
| Duration of tinnitus (mean±SD) | 5.3 ±3.07 years |
| Tinnitus Laterality | Unilateral 47.2% (n=50) |
| Bilateral 52.8% (n=56) | |
| Tinnitus Character | Intermittent 31.1% (n=33) |
| Persistent 68.9% (n=73) | |
| Perception of Tinnitus | Low pitch 41.5 % (n=44) |
| High pitch 33% (n=35) | |
| Ringing 11.3% (n=12) | |
| Humming 14.2% (n=15) |
Table 1: Demographic description and clinical characteristics of tinnitus.
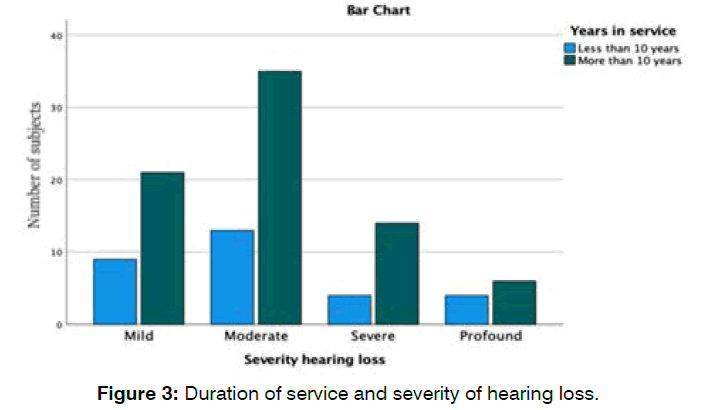
Figure 3 showed more subjects with varying degrees of hearing loss after more than 10 years in service in which most of our subjects (n=35) has moderate degree of hearing loss.
Figure 3: Duration of service and severity of hearing loss.
Overall mean score for Total THI was 27.7, suggesting that majority of our subjects only felt mild handicap due to their tinnitus. 28.3% had slight or no handicap, 41.5% had mild handicap and 30.2% had severe handicap. Individual THI subdomain mean scores shows that the functional subdomain (17.8) affects subjects the most as compared to the emotional (5.7) and catastrophic scores (4.2). Subjects with unilateral tinnitus had a higher mean THI score (59.2) signifying that tinnitus could be more bothersome compared to bilateral tinnitus.
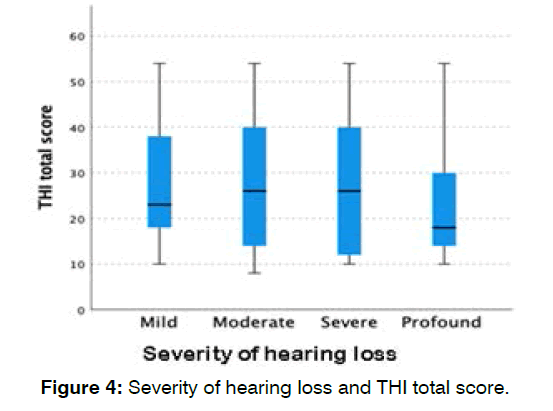
Figure 4 shows equal distribution of total tinnitus handicap scores across all severities of hearing loss indicating that the degree of hearing loss does not affect overall THI scores.
Figure 4: Severity of hearing loss and THI total score.
Table 2 shows the correlation of THI with HADS among army personnel with tinnitus. There was a weak negative correlation between total THI scores and each individual subdomain with HADS anxiety and depression scores. Our result was not statistically significant hence there is no correlation between tinnitus, anxiety, and depression among our subjects. This is due to the lower scores obtained from HADS anxiety and depression scale.
| THI * HADS-A | Spearman’s correlation | Significance |
|---|---|---|
| (2 tailed) | ||
| Total THI * HADS Anxiety | -0.049 | 0.615 |
| THI Functional * HADS Anxiety | -0.031 | 0.752 |
| THI Emotional * HADS Anxiety | -0.027 | 0.78 |
| THI Catastrophic * HADS Anxiety | -0.113 | 0.25 |
| THI*HADS-D | Spearman’s correlation | Significance |
| (2 tailed) | ||
| Total THI * HADS Depression | -0.062 | 0.531 |
| THI Functional * HADS Depression | -0.036 | 0.721 |
| THI Emotional * HADS Depression | -0.02 | 0.835 |
| THI Catastrophic * HADS Depression | -0.032 | 0.747 |
Table 2: Correlation of THI with HADS among subjects with tinnitus.
Discussion
The prevalence of tinnitus is 11.3% among both activeduty army personnel (5.5%) and veterans (5.8%) which reflects the prevalence of tinnitus in general population of the United States which is approximately 1 in 10 adults. Most studies in the western countries show a higher prevalence of tinnitus for males (80%) than females (20%) [19]. There was no comparable survey done locally among army personnel in Malaysia; however, in 1993, there was a cross sectional study done in Selangor, Malaysia [20]. It was to determine the prevalence of hearing loss and hearing impairment among 286 male subjects from a rural area in which the prevalence of symptoms of tinnitus was 19%. In another local study at our university, the prevalence of tinnitus was found to be 33.0% among the otology patients in the outpatient ear, nose and throat clinic, University Kebangsaan Malaysia (UKM) in 2002 [21]. Tinnitus affects up to 30% of army veterans and 15% of active-duty personnel in the United States, [7] that is comparatively 3 times the prevalence of tinnitus which is seen in our study population leading us to think that this could possibly be a case of under reporting of symptoms in our cohort of patients.
There can be many factors that could contribute to anxiety and depression, majority of it could include trauma, stress due to an illness or stress build-up, different traits of personality, having blood relatives with anxiety or depression disorder, drugs, and alcohol. Theories of the severity of tinnitus causing depression and anxiety are well accepted. Functional MRI have shown increased signals in the middle and superior frontal gyri, the cingulate gyrus, the precuneus, and the parietal cortices in tinnitus patients, verified by electroelcephalography and magnetoencephalography studies. Functional imaging studies show that the subgenual Anterior Cingulate Cortex (sgACC) plays an important role in both coping styles [22] and depression [23]. The most recent study by Vanneste et al. showed that tinnitus patients using a maladaptive coping style show increased scores on the THI and experienced louder sounds and more distress in comparison to tinnitus patients using adaptive coping styles [24]. The sgACC and ventromedial prefrontal cortex are considered central dysfunction nodes in depression. The dorsolateral prefrontal cortex has been found to play an important role in anxiety [25]. This evidence further suggests why tinnitus can be associated with major depression, anxiety, and other psychosomatic and/or psychological disturbances.
An alternative theory suggests tinnitus is related to psychological disorders through a cortisol mediator26. Existence of glucocorticoid receptors in the inner ear has been proven, coupled with evidence that tinnitus patients have high cortisol levels which in turn could provoke anxious and depressive symptoms [27]. In 2019, Henry et al reported that 52% of army personnel and veterans with tinnitus were categorized as having anxiety and 21% were classified as having depression in which their subjects reported to have Post-Traumatic Stress Disorder (PTSD) from active combat missions due to tinnitus [28]. In contrast, our study showed only 4.71% were suffering from anxiety and none from depression. Our military soldiers are mainly stationed in peacekeeping missions rather than in the combat field which we postulate that the tinnitus selfretraining therapy to be manageable without dealing with PTSD. Majority of our subjects have persistent (70%) type of tinnitus which was similar to Henry et al. group which reported (77%) of tinnitus to be constant [28].
Army personnel are exposed to noise which could later cause Noise Induce Hearing Loss (NIHL). Other factors that contribute to the acceleration of NIHL and related tinnitus might include smoking, diabetes, and low levels of exercise, as well as non-modifiable factors such as aging, genetics and racial or ethnic influences [29]. These factors should also be considered as it was not done in both Henry et al and our study. The functional (17.79 ± 10.3) subdomain of THI affected subjects the most as compared to the emotional (5.70 ± 10.3) and catastrophic scores (4.21 ± 2.30). This is evidenced by lower HADS-A (4.75 ± 1.83) and HADS-D (2.98 ± 1.21) as it did not affect the subjects THI-emotional and THI-catastrophic scores. This in turn could affect concentration, alertness, and the ability to carry out assigned tasks especially in combat situations [15].
In our study, there was also no association between the degree of hearing loss and their discomfort caused by tinnitus based on THI score. Several studies have tried to show the possible association between THI questionnaire scores and degree of hearing loss [30,31] however, the results have been different and sometimes contradictory. Rajguru et al reported that tinnitus from noise-induced hearing loss in military aircrew can cause fear to crewmembers to be downgraded from their flying duties [32]. There is also a clear association between shooting and hearing loss based on the asymmetry of the loss with right-handed firers having greatest loss in the ear closest to the muzzle which is the left ear [33]. Although hearing protection is routinely supplied to military personnel, it is often not used in active service because of the need to hear warning signals and instructions. Hence, NIHL among military personnel remains a serious problem [34]. Our study limitations were a relatively small sample size (n=106) as compared to studies done abroad ranging from 200- 300 subjects and single centre study as compared to multicentric. It is also unknown to what extent participants felt comfor reporting the presence of tinnitus and the impact of tinnitus on their lives.
Conclusion
Tinnitus can occur in all degrees of hearing loss, and it is associated with poor functional THI scores. There is association of tinnitus with anxiety but not depression among army personnel. These findings suggest that tinnitus should be addressed by healthcare providers in the military in order to maximise functionality and quality of life among our nation’s active-duty army personnel and veterans.
References
- Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990;8(4):221-54.
- Bhimrao SK, Masterson L, Baguley D. Systematic review of management strategies for middle ear myoclonus. Otolaryngol-Head and Neck Surg. 2012;146(5):698-706.
- Stobik C, Weber RK, Münte TF, Walter M, Frommer J. Evidence of psychosomatic influences in compensated and decompensated tinnitus: evidencia de influencias psicosomáticas en acúfenos compensados y descompensados. Int J Audiol. 2005;44(6):370-8.
- Rojas R, Palacios E, D'Antonio M, Correa G. Aberrant internal carotid artery as a cause of pulsatile tinnitus and an intratympanic mass. Ear, Nose & Throat J. 2003;82(3):173-4.
- Sindhusake D, Golding M, Wigney D, Newall P, Jakobsen K, Mitchell P. Factors predicting severity of tinnitus: a population-based assessment. J Am Academy of Audiol. 2004;15(04):269-80.
- Henry JA., Dennis KC, Schechter MA. General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 2005;48:1204-35.
- Zenner HP. A systematic classification of tinnitus generator mechanisms. The int Tinnitus J. 1998;4(2):109-13.
- Sereda M, Hall DA, Bosnyak DJ, Edmondson-Jones M, Roberts LE, Adjamian P, et al. Re-examining the relationship between audiometric profile and tinnitus pitch. Int J Audiol. 2011;50(5):303-12.
- Noreña AJ, Farley BJ. Tinnitus-related neural activity: theories of generation, propagation, and centralization. Hearing Res. 2013;295:161-71.
- Shore S, Zhou J, Koehler S. Neural mechanisms underlying somatic tinnitus. Progress in brain Res. 2007;166:107-548.
- Salviati M, Bersani FS, Terlizzi S, Melcore C, Panico R, Romano GF, et al. Tinnitus: clinical experience of the psychosomatic connection. Neuropsychiatric Disease and Treatment. 2014;10:267.
- Harrop-Griffiths J, Katon W, Dobie R, Sakai C, Russo J. Chronic tinnitus: association with psychiatric diagnoses. J Psychosomatic Res. 1987;31(5):613-21.
- Georgiewa P, Klapp BF, Fischer F, Reisshauer A, Juckel G, Frommer J, et al. An integrative model of developing tinnitus based on recent neurobiological findings. Med Hypotheses. 2006;66(3):592-600.
- Folmer RL, Theodoroff SM, Martin WH, Shi Y. Experimental, controversial, and futuristic treatments for chronic tinnitus. J Am Acad of Audiol. 2014;25(01):106-25.
- Yankaskas K. Prelude: noise-induced tinnitus and hearing loss in the military. Hearing Res. 2013;295:3-8.
- Aziz, Syed, Syed H. Factors Influencing Safety Behavior in the Malaysian Army. Diss. Universiti Utara Malaysia, 2012.
- Ewe S, Ishak WS. The Tinnitus Handicap Inventory & Mini-Tinnitus Questionnaires: Reliability & Validity of the Malay Version. Int Med J. 2019;26(6).
- Yahya F, Othman Z. Validation of the Malay version of hospital anxiety and depression scale (HADS) in Hospital Universiti Sains Malaysia. Int Med J. 2015;22(2):80-2.
- McCormack A, Edmondson-Jones M, Somerset S, Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hearing Res. 2016;337:70-9.
- Hassim N, Rampal KG. Prevalence of hearing loss and hearing impairment among rural males in Selangor. The Med J Malaysia. 1994;49(1):78-85.
- Ali A. Evaluation of audiological rehabilitation services for adults with hearing impairment in Malaysia. 2004.
- Kross E, Davidson M, Weber J, Ochsner K. Coping with emotions past: the neural bases of regulating affect associated with negative autobiographical memories. Biological psychiatr. 2009;65(5):361-6.
- Drevets WC, Price JL, Furey ML. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Structure and Function. 2008;213(1):93-118.
- Vanneste S, Joos K, Langguth B, To WT, De Ridder D. Neuronal correlates of maladaptive coping: An EEG-study in tinnitus patients. PLoS One. 2014;9(2):e88253.
- Fregni F, Marcondes R, Boggio PS, Marcolin MA, Rigonatti SP, Sanchez TG, et al. Transient tinnitus suppression induced by repetitive transcranial magnetic stimulation and transcranial direct current stimulation. Eur J Neurol. 2006;13(9):996-1001.
- Hébert S, Paiement P, Lupien SJ. A physiological correlate for the intolerance to both internal and external sounds. Hearing Res. 2004;190(1-2):1-9.
- Rarey KE, Curtis LM. Receptors for glucocorticoids in the human inner ear. Otolaryngol Head Neck Surg. 1996;115(1):38-41
- Henry JA, Griest SE, Blankenship C, Thielman EJ, Theodoroff SM, Hammill T, et al. Impact of tinnitus on military service members. Military Med. 2019;184(1):604-14.
- Imam L, Hannan SA. Noise-induced hearing loss: a modern epidemic?. British J Hospital Med. 2017;78(5):286-90.
- Ratnayake SA, Jayarajan V, Bartlett J. Could an underlying hearing loss be a significant factor in the handicap caused by tinnitus?. Noise and Health. 2009;11(44):156.
- Savastano M. Tinnitus with or without hearing loss: are its characteristics different?. Eur Arch Oto-Rhino-Laryngol. 2008;265(11):1295-300.
- Rajguru R. Military aircrew and noise-induced hearing loss: prevention and management. Aviation, Space, and Environ Med. 2013;84(12):1268-76.
- Chung DY, Gannon RP, Willson GN, Mason K. Shooting, sensorineural hearing loss, and workers' compensation. J Occupational Med. 1981:481-4. Themann CL, Masterson EA. Occupational noise exposure: A review of its effects, epidemiology, and impact with recommendations for reducing its burden. The J the Acoustical Society of Am. 2019;146(5):3879-905.
1Department of Otorhinolaryngology and Head and Neck Surgery, Level 9, Clinical Block, Hospital Canselor Tuanku Mukhriz, Universiti Kebangsaan Malaysia Medical Center, Jalan Yaacob Latiff, 56000 Cheras, Kuala Lumpur, Malaysia.
2Center of Ear, Hearing and Speech (Institute-HEARS), Faculty of Health & Sciences, Universiti Kebangsaan Malaysia, 56000 Kuala Lumpur, Malaysia
3Department of Otorhinolaryngology and Head and Neck Surgery. Hospital Angkatan Tentera Tuanku Mizan
4Department of Community Health, Medical Faculty, Universiti Kebangsaan Malaysia
5Department of Psychiatry, Hospital Canselor Tuanku Mukhriz, Universiti Kebangsaan Malaysia Medical Center
Send correspondence to:
Reuben Thomas
Department of Otorhinolaryngology and Head and Neck Surgery, Level 9, Clinical Block, Hospital Canselor Tuanku Mukhriz, Universiti Kebangsaan Malaysia Medical Center, Jalan Yaacob Latiff, 56000 Cheras, Kuala Lumpur, Malaysia, E-mail: reubencrm@gmail.com
Paper submitted on April 16, 2022; and Accepted on May 24, 2022
Citation: Reuben Thomas, Asma A, Noor Dina H, Loh Sheau Torng, Aniza Ismail, Shalisah Sharip. Association of Tinnitus with Anxiety and Depression among Active-Duty Army Personnel and Veterans at Hospital Angkatan Tentera Tuanku Mizan, Malaysia. 2022;26(1): 68-74