The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 24, Issue 1 / June 2020
Research Article Pages:1-6
Clinical and morphological results of xenografts to use in myringoplasty
Authors: Botirov AJ, Isroilov RI, Matkuliyev KHM, Khasanov US. Khodjanov SH, Akhundjanov NO, Djuraev JA, Shaumarov AZ, Akhmedov SE, Khaydarova GS, Zokirova ZJ
PDF
Abstract
The main aim of our study was to study morphological state of the autograft from the fascia of the temporal muscle in myringoplasty. Until now, there is no consensus on issue of which fabrics are more suitable for use in the eardrum. We decided to study of use of an autograft from the fascia of the temporal muscle for myringoplasty in rabbits in the experiment, and in patients with chronic dry mesotympanitis. An electron microscopic examination of the fascia taken immediately, after 10, 20 min and 1 h after sampling. It was found that there are no gross destructive changes in the fascia structure. Minor changes are detected in the form of a light disorganization of the collagen complex, granular dystrophy with an increase in cell. Inflammatory diseases of the middle ear are widespread among population of all age groups. In the experiment, a positive result was obtained in 29 (82.8%) rabbits. In our research we performed morphological features of xenograft engraftment in an experimental animal on 3, 7, 14, 21 days and 1-3 months. In period from 3 days to 3 months after operation, the animals were euthanized by an air embolism and subjected to pathological examination. Then recovered xenograft, was examined macro and microscopically. Pieces were fixed in a 10% solution of neutral formalin. After washing with water, dehydration was carried out in alcohol and chloroform, and after, waxed with paraffin. Histological sections were stained with hematoxylin-eosin. Collagen fibers were detected by method of Vann-Gieson
Keywords: Myringoplasty, fascia, eardrum, auto graft, muscle
Introduction
Closing the perforation of the tympanic membrane eliminates of anatomical defect, prevents recurrence of inflammatory process in the middle ear, and prevents development of sensorineural hearing loss or other complications [1-6] . For the first time in 1879, Bertold used a skin flap from his forearm in clinical practice to restore the eardrum [7-15] . For a long time, skin flaps remained the material of choice for closing defects in the eardrum [8-13] . According to skin flap without inflammatory changes in follow-up period up to 5 years after surgery was observed in 57% of patients14, in 43% of the plastic flap had certain defects and did not fulfill of main function of the eardrum. In long term after surgery, hearing loss in area of speech frequencies less than 40 dB was in 62.2% of patients, less than 30 dB in 40.2% of patients [15-17] covered the eardrum defect with a free skin graft from the ear region near an earlobe. The flap was thinned and laid on prepared bed, completely covering of perforation and epidermal edge of the eardrum [18] . Recommends use of a skin flap for marginal and small central perforations of the tympanic membrane. In 40 patients with myringoplasty [19] closed the eardrum defect with a free skin graft from behind the ear area. Complete graft engraftment was observed in 24 patients. With the development of oto-surgery, clinicians began to use more effective meatal and meato-tympanal flaps to restore integrity of the eardrum. In patients with chronic mesotympanitis used meato-tympanal flaps to close the defects of the eardrum in posterior quadrants, data are presented on an effectiveness of closing small defects of the tympanic membrane in posterior quadrants by displacement of formed meato-tympanal flap created a wound surface at edges of the eardrum defect and subsequently used a posterior meatal flap to close it. According to large defects of the eardrum, mucocutaneous flaps consisting of the skin of external auditory canal and implanted mucous membrane of cheek are effective. In course of long-term clinical observations of use of a skin graft and a flap on pedicle during myringoplasty, following shortcomings were revealed: presence of highly differentiated epithelium, glandular appendages led to formation of epidermal cysts, cholesteatoma and development of allergic reactions [6] . Severity of the thick layer of collagen and elastic fibers made it difficult to lay, caused contraction and tucking of edges of the flap, leading to malnutrition, followed by atrophy and necrosis [18-20] . Many surgeons have an opinion about him as a graft of little use for myringoplasty. The main disadvantage limiting its use is the presence of a highly differentiated epithelium and glandular appendages. As clinical experience has shown, these features often lead to necrosis or atrophy, formation of epidermal cysts and cholesteotomas. In addition, the flap needs to be neatly laid (side to side), which is sometimes difficult to perform because of its pronounced ability to contract and twist the edges due to presence of a powerful elastic and collagen layer [21] . Currently, free skin flaps are independently used in exceptional cases, and more often as flaps that complement other plastic tissues. Not found widespread and skin rags on the leg, cut from the ear region. Only acceptable type of skin graft is a flap on leg, formed from the skin of external auditory meatus, which does not contain sebaceous and sweat glands and has a common blood vessel network. But it cannot be used to close large perforations without additional tissue, otherwise the membrane formed from it will be thin and atrophic [22] . Significant difficulties due to the biological characteristics of skin grafts forced otosurgeons to begin searching for new materials to replace the eardrum defect from less differentiated tissues, which have a low metabolic rate and, therefore, are more stable under conditions of low nutrition, are more tolerant to infection and less undergo changes engraftment compared to skin [23] . These circumstances dictated the need to search for plastic materials for myringoplasty from less differentiated tissues. Tissues of mesenchymal genesis appeared to be more preferable for these purposes. Transplants from less differentiated tissue of mesodermal origin (fascia, vein, periosteum, adipose tissue) have a low metabolic rate and undergo engraftment undergo less changes compared to the skin [24] . Widespread and generally recognized among clinicians as plastic material for restoring the integrity of the eardrum was the fascia of the temporal muscle [22-25] . Experimental studies have shown that epiphasia of the temporal muscle has the ability to produce epithelial cells and bears the least differences in sound transmission compared to normal. Currently, the fascia of the temporal muscle is successfully used for small and large defects of the eardrum. When analyzing long-term clinical results, optimal engraftment is achieved in 80-93% of cases [16] . Along with the fascia of the temporal muscle, otosurgeons for the reconstruction of the tympanic membrane successfully used the fascia of the thigh and foot [11] , lower leg [7-10] . With myringoplasty in patients with chronic mesotympanitis, the vein wall [7] , periosteum [5] and a fat auto graft were successfully used [18] . Allografts from the dura mater of an adult and a fetus [21] , an allograft of the tympanic membrane. In studies of information is given on the plasty of extensive defects with an allograft of the tympanic membrane along with a hammer and a dura mater. Many years of clinical experience with use of these grafts during surgical interventions on the middle ear revealed a number of disadvantages rejection of plastic material, recurrence of perforation in a non-tympanic membrane, the need for additional operations to collect the transplant, which negatively affects the anatomical and functional results of surgical treatment of patients. Therefore, in modern otosurgery, the development of new highly effective transplants for the repair of eardrum defects is an urgent and important problem.
Materials and Methods
We observed 110 patients with chronic purulent otitis media who underwent surgery from 2015 to 2019. According to a clinical and functional study, it was found that 42 patients (38.2%) had total and 68 patients (61.8%) subtotal perforation of the eardrum. The mucous membrane of the medial wall of the tympanic cavity in all patients was pale pink with no signs of epidermization. In 17 patients (15.4%), it was thickened due to swollen (edema). In 10 patients (9.1%), the humidity of the mucous membrane of the tympanic cavity was noted. The period of “dry ear” before the time of surgery ranged from 2-6 months, an average of 106 days. The ventilation function of the auditory tube was evaluated as 1 degree - in 26 patients (23.6%), 2 - in 31 (28.2%), 3 - in 22 (20%), 4 - in 20 (18.2%), 5 - in 11 (10%). Drainage function in 36 patients (32.7%) was of 1 degree, in 49 (44.5%) - 2, in 25 (22.8%) - 3. The age of patients ranged from 18 to 60 years. Women were 58 (52.7%), men 52 (47.3%). A socially adequate level of hearing was in 63.6% of patients from group 1, in 62% from group 2. Operations were performed under general anesthesia (endotracheal anesthesia). Used micro-instruments, motor system, microscope "Carl Zeiss Surgical GmbH". After access to the structures of the middle ear, an audit of its spaces was performed. Remediation activities were carried out if necessary. We started reconstruction. Sizes of the eardrum defect, the condition of the auditory osicles, and the mucous membrane of the tympanic cavity were evaluated. The significance of differences between the studied groups was determined by calculating the student t-test. Differences in the compared values were considered significant at a significance level of p<0.05.
Results and Discussion
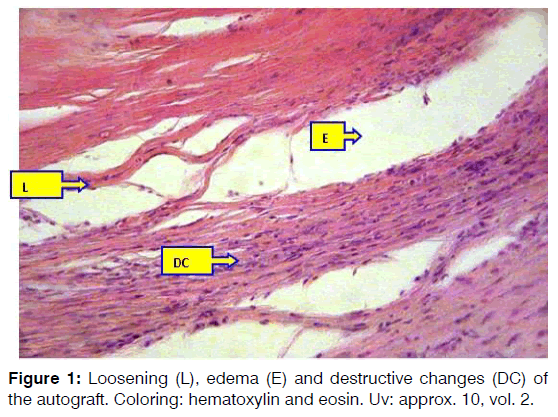
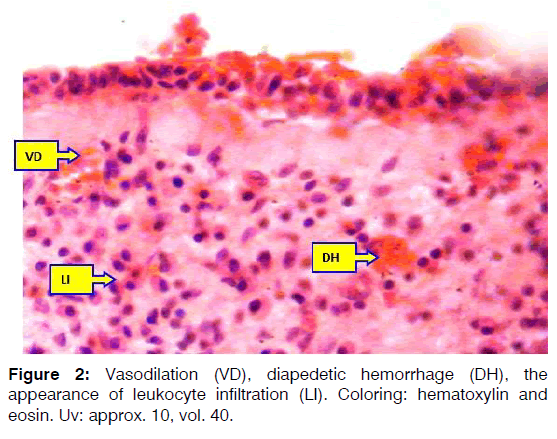
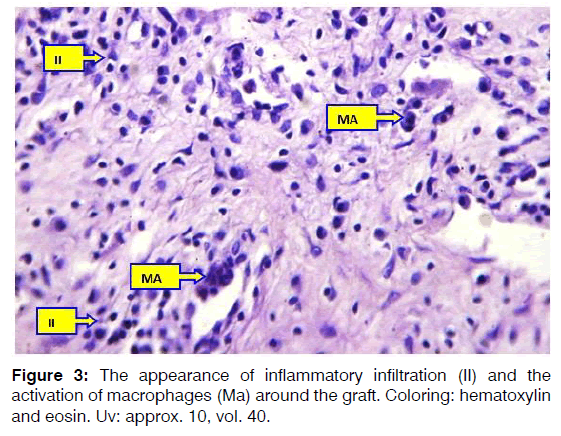
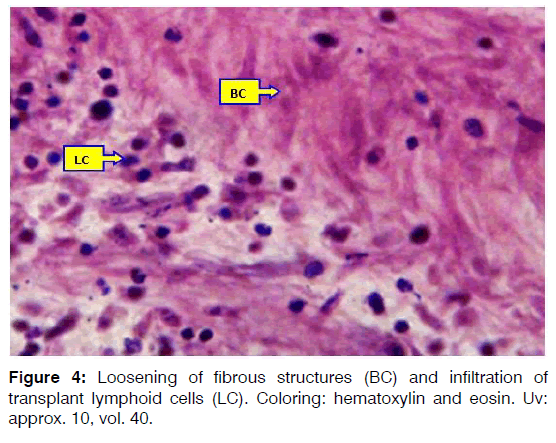
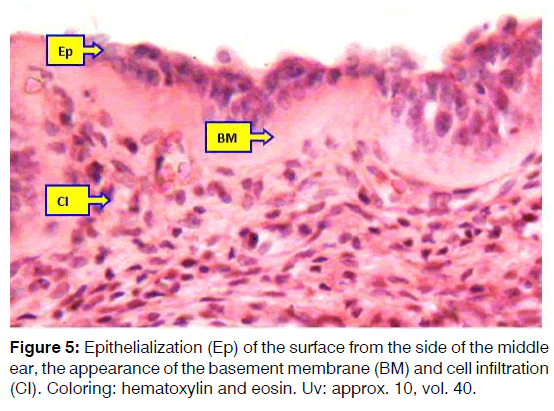
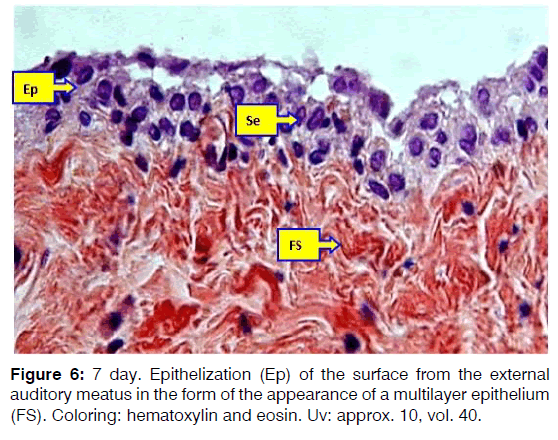
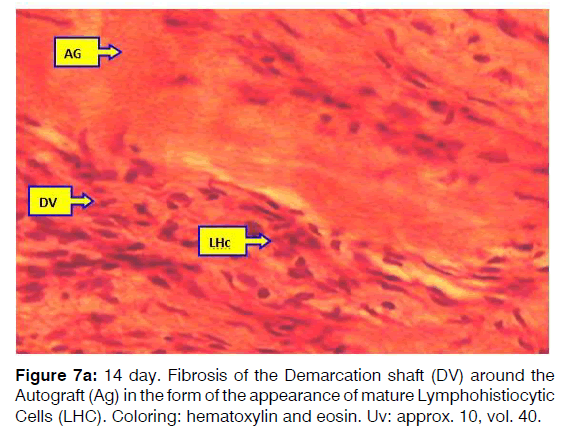
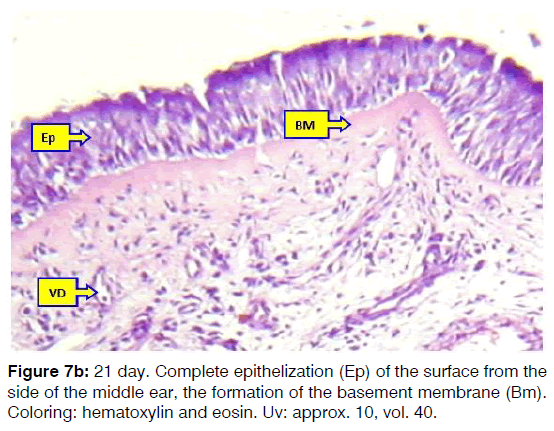
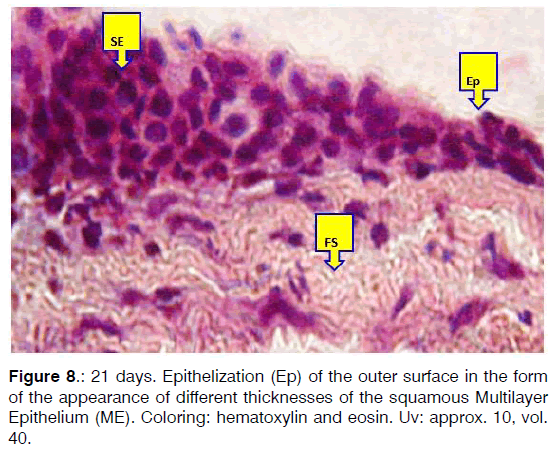
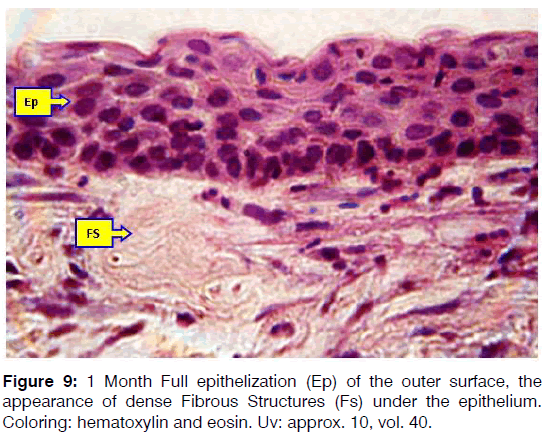
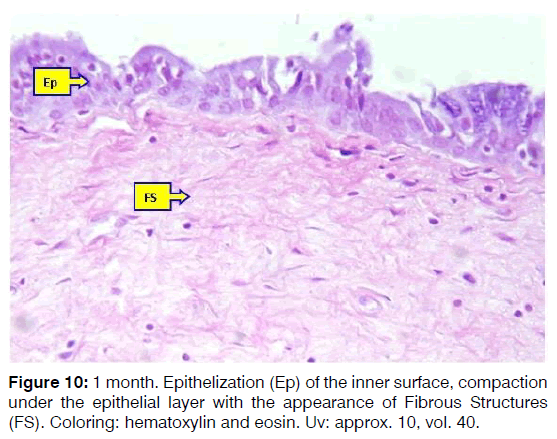
On day 3 after autograft grafting in the tympanic membrane after modeling of chronic otitis media, discirculatory, destructive changes were detected around the graft. Destructive changes were manifested by traumatic loosening and thinning of soft tissues (Figure 1), in the thickness of which the development of hemorrhages and thrombosis was noted. The fascia tissue during this period of the experiment is somewhat loosened with loss of stainability of the fibrous structures in the form of blanching and hypochromasia of the protein component of the fascia due to interfiber edema and disorganization of the interstructural substance. Around the planted fascia, vasodilation of the mainly microvasculature and venules is noted. Moreover, the vessels are dilated, thin-walled with perivascular edema and diapedetic hemorrhage (Figure 2). In the lumen of blood vessels, mainly post-capillary venules, there is a peripheral arrangement of leukocytes and monocytes with migration into the surrounding tissue through a transendothelial transition. And around destructively altered tissue masses macrophages with high phagocytic activity appear (Figure 3). On the 7th day of the experiment, the formation of a demarcation inflammatory infiltrate around the implanted autologic fascia in the area of the chronically inflamed eardrum was noted. This demarcation shaft was represented by the majority of dilated thin-walled vessels, lymphohistiocytic cell elements, active macrophages, giant macrophages of foreign bodies and randomly located argyrophilic and reticular fibers (Figure 4). During the given period of the experiment, from the side of the planted fascia, there was some thinning and a decrease in edematousdestructive changes. On the periphery of the fascia, on both sides, the fibrous structures of the fascia merge and intertwine with the cellular-fibrous elements of the surrounding demarcation shaft. The middle part of the fascia remains dense and fibrous, only single mononuclear cells penetrate the thickness of the fibrous structures, but blood vessels do not form. From the side of the middle ear, during this period of the experiment, enhanced epithelization of the surface of the planted fascia is noted. At the same time, the fact is determined that, at the periphery of the autograft, the integumentary epithelium initially becomes multirow and hyperchromic, then the regenerative activity of the epithelium increases and epithelization of the autograft surface occurs (Figure 5). From the side of the outer ear, epithelization is relatively slower. Acanthosis and parakeratosis occur in the multilayer integument epithelium. The acanthotic epithelium shifts towards the surface of the autograft; epithelization occurs in the form of the appearance of initially a single-layered, then a multilayer epithelium (Figure 6). On the 14th and 21st day of the experiment, the implanted autologic fascia fully merges with the surrounding soft tissues. Around the autograft, the demarcation shaft becomes more mature and consists of cell-fibrous tissue (Figure 7a). In the composition of which the vessels are reduced and the available vessels are relatively narrowed and without discirculatory disorders. Only directly in the circumference of the fibrous structures of the planted fascia is the preservation of single lymphoid and macrophage cells observed. The middle part of the autograft at this time of the experiment is compacted, the fibrous structures are homogenized without swelling and loosening. On both sides, the surface of the autograft is completely epithelized. From the side of the middle ear, a multi-row prismatic epithelium appears with the formation of a basement membrane and a vascular submucosal layer (Figure 7b). On the surface from the side of the external auditory meatus, a stratified squamous epithelium of different thickness is formed (Figure 8). The results of the morphological study showed that 1 month after replanting the autologous fascia in the area of the tympanic membrane against the background of chronic otitis media, complete fusion of the fascia with the surrounding soft tissues was noted. From the side of the external auditory meatus, complete epithelization was noted with the development of a complete multilayer squamous epithelium on the surface of the autograft (Figure 9). On the inside of the graft, the development on the surface of a full-fledged multi-row prismatic epithelium is also revealed. Under the epithelium, the basement membrane remains somewhat thickened and uneven and appears to be a homogeneous eosinophilic mass (Figure 10). Only under the basement membrane, in the circumference of the autologous fascia, is the preservation of certain cellular elements of macrophage and fibrocystic origin. Middle part of the planted fascia becomes even denser and homogeneous without any cellular elements and vascular formations 3 months after replanting the autologic fascia in the region of the tympanic membrane against the background of simulated chronic otitis media, the fact is noted that in the fascia implantation zone all cell-tissue elements are indistinguishable from normal intact tissue. From the side of the external auditory canal, the integumentary epithelium is represented by a stratified squamous epithelium, which consists of uniformly spaced layers of squamous epithelium, on the surface of a small amount of horny substance. From the side of the middle ear, the integumentary epithelium is represented by normal multirow prismatic cells. On both sides, under the epithelial basement membrane and its own connective tissue membrane, a thin layer of homogeneous fibrous tissue is presented. Structural elements of implanted autologic fascia in stainability and fibrous elements do not differ from the surrounding normal tissue. Almost reactive changes are not detected in the fascia circumference, there are few vessels and are represented by arterioles and capillaries.
Conclusions
Thus, based on the survey data, it could be concluded that Results of a morphological study in dynamics after replanting an aerologic fascia in the tympanic membrane against a background of simulated chronic otitis media showed that early reactive destructive, dis circulatory and acute inflammatory changes develop around the auto graft with development of an inflammatory demarcation shaft from thin-walled vessels by 7th day, young cell elements of mainly lympho-histiocytic, monocyte-macrophage origin. But the cellular elements of the demarcation shaft do not penetrate into the thickness of the planted fascia, only surround from different sides. As part of the fascia in the early stages of the experiment, there is a slight swelling and loosening of the fibrous structures. By 14th day of the experiment, these acute destructive and inflammatory changes stabilize and on the 21st day turn into mature connective tissue structures. At this time, complete epithelization of the surface with the development of the corresponding integumentary epithelium for each part of the ear is noted on both sides of the auto graft. in subsequent periods, the disappearance of discirculatory and inflammatory changes in the composition of the healing tissue and the formation of the integument epithelium, basement membrane, sub mucosal layer and fibrous structures of the tympanic membrane are noted.
Conflict of Interest
The authors declare no conflict of interest.
References
- Hassan MH. Fat graft myringoplasty: A prospective clinical study, Egyptian J Ear, Nose, Throat and Allied Sciences. 2013;14:91-5.
- Nemer Al-K, Mohammad AH. Myringoplasty in children retrospective analysis of 35 cases, Braz. J Otorhinolaryngo. 2009;75:371-4.
- Moustafa H, Mohammed G. Nasal septal perichondrium versus temporalis fascia in transmeatal myringoplasty, Egyptian J Ear, Nose, Throat and Allied Sciences. 2011;12:1-6.
- Omran AA. Endoscopic bivalve inlay cartilage myringoplasty for central perforations: Preliminary report, Egyptian J Ear, Nose, Throat and Allied Sciences. 2012;13:37-42.
- Zhengcai L. The outer diameter of the endoscope is important when performing endoscopic transcanal myringoplasty, Braz. J Otorhinolaryngo. 2017;83:730-1.
- Amit S, Munish S, Gaveshna G. Endoscopic transcanal myringoplasty: Is learning curve a myth?, Journal of Otology. 2018;13:101-4.
- Rachel E, Angus W. Revisiting an old technique: Local anaesthetic for myringoplasties, International Journal of Surgery. 2014;12:1-40.
- Vincent NA. A Technique of anaesthesia for the operations of myringoplasty and tympanoplasty, Brit J Anaesth. 1958;30:380-2.
- Zhengcai L. Treatment of tympanic membrane perforation using bacterial cellulose: A randomized controlled trial, Braz J Otorhinolaryngol. 2016;82:618-19.
- Zhengcai L. The effect of epidermal growth factor on the pseudo-healing of traumatic tympanic membrane perforations, Braz J Otorhinolaryngol. 2019:6:1-4.
- Tawab HM. Fadi MG, Tariq MA, Louay S. Myringoplasty with and without cortical mastoidectomy in treatment of non-cholesteatomatous chronic otitis media: a comparative study, Clin Med Insights: Ear, Nose and Throat. 2014;1:179-80.
- Santosh UP, Prashanth KB, Rao MS. Study of myringoplasty in wet and dry ears in mucosal type of chronic otitis media, J Clin and Diagnos Res. 2016;1:4-6.
- Sangavi AKB. Assessment of hearing improvement by myringoplasty, J Scientific and Innovative Res. 2015;4:67-70.
- Gaur RS, Tejavath P, Swati C. Comparative study of microscopic-assisted and endoscopic-assisted myringoplasty. Indian J Otology. 2016;22:177-82.
- Shekharappa MK, Shruthi SM. Cartilage Myringoplasty: An Ideal Grafting Technique for Complex Perforations, J Clin Diagnostic Res. 2017;11:102-64.
- Furukawa M. Surgical management of myringosclerosis over an entire perforated tympanic membrane by simple underlay myringoplasty. Int Journal Otolaryngology. 2016;1:1-8.
- Murugendrappa MA, Naganahalli S, Shambulingegowda A, Basavaraj GP. Comparative study of two different myringoplasty techniques in mucosal type of chronic otitis media, J Clin Diagn Res. 2016;10:1-3.
- Kulkarni V, Mittal M. Single Flap Otoendoscopic Myringoplasty for Large Central Perforation-A Pilot Study, Int J Otolaryngology and Head & Neck Surgery. 2014;1:3-161.
- Alhabib SF, Saliba I. Hyaluronic acid fat graft myringoplasty versus autologous platelet rich plasma, J Clin Med Res. 2017;9:30-34.
- Choi SH, Song HY, Song CI. Fibrinogen-based collagen fleece graft myringoplasty for traumatic tympanic membrane perforation, J Audiol Otol. 2016;20:139-145.
- Sharma C, Jagat S, Kakkar V, Priya M, Surender B. Fat graft myringoplasty in small central perforations. Indian J Otol. 2014;20:211-15.
- Lee DH, Kim J, Shin E, Kim Y, Cho Y. Clinical Analysis of Paper Patch Myringoplasty in Patients with Tympanic Membrane Perforations, J Int Adv Otol. 2016;12:142-6.
- Kalsotra P, Gupta R, Gupta N, Kotwal S, Suri A, Kanotra S. Overlay versus underlay myringoplasty: A comparative study, Ind J Otol. 2014;20:183-8.
- Panchal V, Joginder SG, Sharad H, Bhushan K, Kaintura M. To evaluate and compare the results of over-underlay graft technique with conventional underlay myringoplasty, Ind J Otol. 2015;21:274-9.
- Kaushik S, Jain R. A study of the role of tissue adhesives in myringoplasty, J Evolution of Medical and Dental Sci. 2017;25:2101-4.
Department of Otolaryngology and Stomatology, Tashkent Medical Academy, Uzbekistan
Send correspondence to: Abdukakharovic DJ Department of Otolaryngology and Stomatology, Tashkent Medical Academy, Uzbekistan, Email: drdjuraev@mail.ru Phone: +998974000351
Paper submitted to the ITJ on December 16, 2019; and accepted on January 06, 2020.
Citation: Clinical and morphological results of xenografts to use in myringoplasty. 24(1):1-6