The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 27, Issue 2 / December 2023
Research Article Pages:135-140
10.5935/0946-5448.20230021
Does the Location of a Small Tympanic Membrane Perforation Affect the Dgree of Hearing Loss in Adult Patients with Inactive Mucosal Chronic Suppurative Otitis Media?
Authors: Ahmed Muhei Rasheed
PDF
Abstract
Background: Tympanic membrane perforation due to inactive mucosal chronic suppurative otitis media is a common problem in otolaryngology, with consequent conductive hearing loss. Still, there is controversy about the relationship between the location of the tympanic membrane perforation and the degree of hearing impairment. Aim of the study: To assess the correlation between the location of a small tympanic membrane perforation and the degree of conductive hearing loss in adult patients with inactive mucosal chronic suppurative otitis media. Patients and Methods: A prospective cross-sectional study enrolled 74 adult patients with small tympanic membrane perforations (perforation involves less than one quadrant of the tympanic membrane) and conductive hearing loss (air-bone gap ≥ 20 dB HL) due to inactive mucosal chronic suppurative otitis media for at least 3 months. The locations of the tympanic membrane perforations were classified as anterosuperior, anteroinferior, posterosuperior, and poster inferior perforations. Audiometric analysis and a CT scan of the temporal bone were done for all patients. The means of the air and bone conduction pure tone hearing threshold averages at frequencies 500, 1000, 2000, and 4000 Hz were calculated, and consequently, the air-bone gaps were calculated and presented as means. The ANOVA test was used to compare the means of the air-bone gaps, and the Scheffe test was used to determine if there were statistically significant differences regarding the degree of conductive hearing loss in relation to different locations of the tympanic membrane perforation. Results: The ages of the patients ranged from 20 to 43 years (mean = 31.9 ± 6.5 years), of whom 43 (58%) were females and 31 (42%) were males. The means of the air-bone gaps were 32.29 ± 5.41 dB HL, 31.34 ± 4.12 dB HL, 29.87 ± 3.48 dB HL, and 29.30 ± 4.60 dB HL in the posteroinferior, posterosuperior, anteroinferior, and anterosuperior perforations, respectively. Although the air-bone gap's mean was greater in the posteroinferior perforation, statistical analysis showed that it was insignificant (P-value=0.168). Conclusion: In adult patients with inactive chronic suppurative otitis media, the anteroinferior quadrant is the most common location of the tympanic membrane perforation, and there was an insignificant correlation between the location of a small tympanic membrane perforation and the degree of conductive hearing loss.
Keywords: Tympanic membrane perforation, Inactive mucosal chronic suppurative otitis media, Audiogram, Conductive hearing loss, Air-bone gap.
Introduction
Supperative and non-supurative otitis media are common causes of hearing impairment [1-4]. Chronic Suppurative Otitis Media (CSOM) is characterized by aural discharge through a perforated Tympanic Membrane (TM) for a period of two to six weeks [5]. Depending on the coexistence of cholesteatoma, CSOM is classified into safe and unsafe types [6]. The common causes of TM perforation include acute suppurative otitis media, CSOM, and trauma [7].
Chronic suppurative otitis media affects about 0.5% of the population, so it is a common cause of TM perforation [8]. Hearing loss is a decline in hearing ability that ranges from minimum to maximum loss [9]. Clark grading system was used to classify hearing loss into normal (≤ 15 dB), minimal (16-25 dB), mild (26–40 dB), moderate (41–55 dB), moderately severe (56–70 dB), severe (71–90 dB), and profound (>90 dB) [10]. The hearing loss in CSOM ranges from mild (26 dB) to moderate (up to 55 dB) [11].
Some previous studies showed that the site of the TM perforation affects the level of hearing loss; they showed that the posteriorly located perforations increase the conductive hearing impairment [7, 12-14]. However, the more severe degree of hearing loss was associated with posteroinferior quadrant perforations, but some other studies showed that the degree of hearing impairment was not affected by the site of the TM perforation [15, 16].
However, the effect of the TM perforation on the degree of hearing loss is still controversial. The aim of this study is to assess the correlation between the location of a small tympanic membrane perforation and the degree of conductive hearing loss in adult patients with inactive mucosal CSOM.
Patients and Methods
The current prospective cross-sectional study was conducted in the Otolaryngology Consultant Clinic in the Medical City, Baghdad, Iraq, for the period from March to August 2023. The patients included in this study were adult patients with small TM perforations (small TM perforation: perforation involves less than one quadrant of the TM) and conductive hearing loss; air-bone gap (ABG) ≥ 20 dB HL; due to inactive CSOM for at least 3 months. The air and bone conduction pure tone hearing thresholds at frequencies 500, 1000, 2000, and 4000 Hz were used to calculate the patient’s hearing threshold [17, 18]. Exclusion criteria were large TM perforations, multiple TM perforations, traumatic TM perforations, marginal TM perforations, myringosclerosis, cholesteatoma, sensorineural hearing loss, and a history of previous ear surgery. Patients with chronic diseases that can affect hearing, such as diabetes mellitus, were also excluded from the study.
The total number of patients enrolled in this study was 74. A routine history and otolaryngological examination were performed, including a microscopical and a zero-degree rigid otoscopic ear examination (4mm in diameter and 4.5cm in length). All patients were sent for a CT scan of the temporal bone to assess the ossicles and the mastoid air cell system. The TM was divided during otoscopic examination by two imaginary lines into four quadrants (Anterosuperior AS, anteroinferior AI, posterosuperior PS, and posteroinferior PI); a horizontal line passed through the umbo, and a second vertical line bisects the horizontal line at a right angle, so the locations of the TM perforations were classified as Anterosuperior Perforation (ASP), Anteroinferior Perforation (AIP), Posterosuperior Perforation (PSP), and Posteroinferior Perforation (PIP). Audiometric Analysis (Otometrics, Madsen; Astera) in a sound-treated room at reference frequencies from 250 Hz to 8000 Hz was done for all patients (Figure 1). The means of the air and bone conduction Pure Tone Hearing Threshold Averages (PTHTAs) at frequencies 500, 1000, 2000, and 4000 Hz were calculated, and consequently, the Air Bone Gaps - (ABGs) were calculated and presented as means.
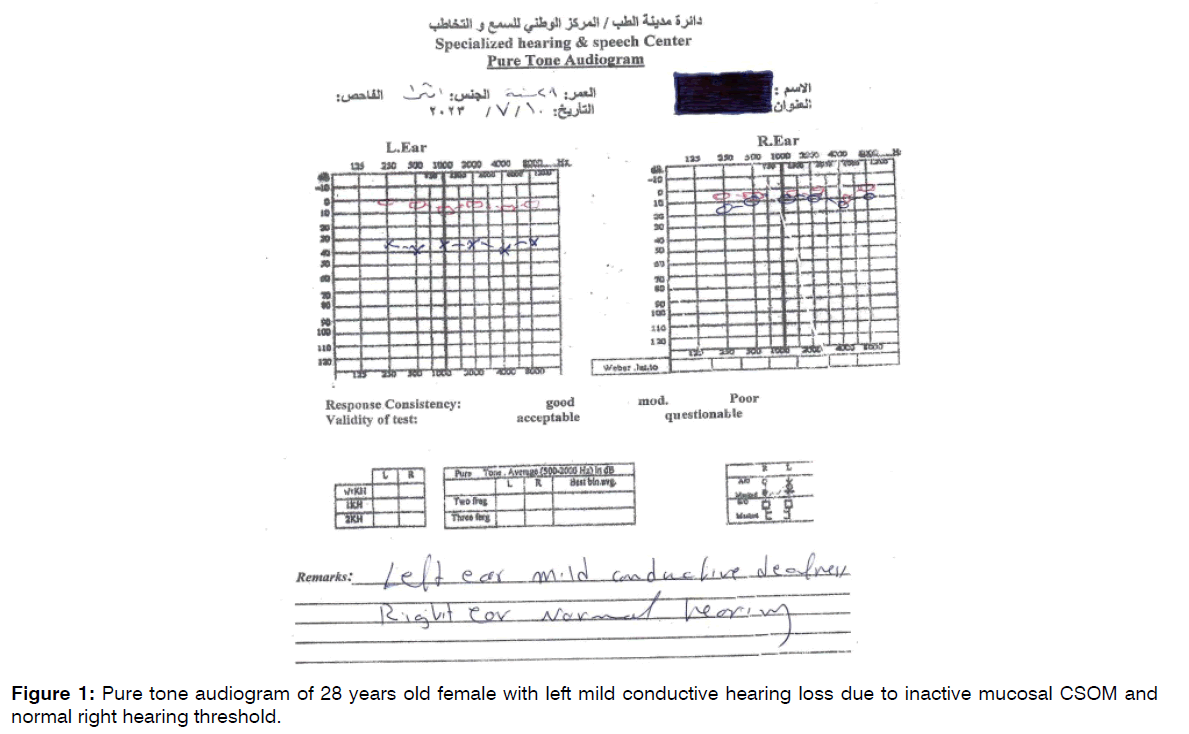
Figure 1: Pure tone audiogram of 28 years old female with left mild conductive hearing loss due to inactive mucosal CSOM and normal right hearing threshold.
The data, presented as ABG’s means, were analyzed statistically using Statistical Package for Social Sciences (SPSS version 23). The ANOVA test was used to compare the means of ABGs, and the Scheffe test was used to determine if there were statistically significant differences regarding the degree of conductive hearing loss in relation to different locations of the tympanic membrane perforation. The confidence level of 95% was set, and a 5% margin of error was accepted. A P-value <0.05 was considered significant. Power analysis was done using G power software; the significance level (ɑ) was 0.05 and the power was 0.8 with a minimal effect. The sample size of 74 will gain a power of 0.803527.
Results
The current study included 74 patients, of whom 43 (58%) were females and 31 (42%) were males. The ages ranged from 20 to 43 years (mean = 31.9 ± 6.5 years), as shown in Table 1.
| Age (years) | Number of patients | Percentages |
|---|---|---|
| 20-29 | 32 | 43.24% |
| 30-39 | 29 | 39.19% |
| 40-45 | 13 | 17.57% |
| Total | 74 | 100% |
Table 1: Age distribution (n=74).
Hearing loss alone was the chief complaint in 64 patients (86.5%), while 10 patients (13.5%) presented with hearing loss and tinnitus. The TM perforations were left-sided in 41 patients (55.4%) and right-sided in 33 patients (44.6%). The anteroinferior quadrant was the most common site of the TM perforations (40.54%). The distribution of the patients according to the location of the TM perforations and the severity of hearing loss is shown in Table 2.
| Location of the tympanic membrane perforation | Mild hearing loss | Moderate hearing loss | Total | ||
|---|---|---|---|---|---|
| Number of patients | Percentages | Number of patients | Percentages | ||
| Anterosuperior perforation | 10 | 13.51% | - | - | 10 (13.51%) |
| Anteroinferior perforation | 27 | 36.49% | 3 | 4.05% | 30 (40.54%) |
| Posterosuperior perforation | 7 | 9.46% | 4 | 5.41% | 11 (14.87%) |
| Posteroinferior perforation | 17 | 22.97% | 6 | 8.11 | 23 (31.08%) |
| Total | 61 | 82.43% | 13 | 17.57% | 74 (100%) |
Table 2: Distribution of the patients according to the location of the TM perforations and the severity of hearing loss (n=74).
Although the PI perforation was associated with the greatest conductive hearing loss (ABG’s mean), it was statistically insignificant (P-value=0.168). The relationship between the location of the TM perforations and the means of the ABGs are shown in Table 3 and Figure 2.
| Location of the tympanic membrane perforation | Air-bone gap's mean ± Std. Deviation (dB HL) | P-value |
|---|---|---|
| Anterosuperior perforation | 29.30±4.60 | 0.168 |
| Anteroinferior perforation | 29.87±3.48 | |
| Posterosuperior perforation | 31.34±4.12 | |
| Posteroinferior perforation | 32.29±5.41 | |
| Total | 30.72±4.42 |
Table 3: Relationship between the location of the TM perforations and the means of the ABGs (n=74).
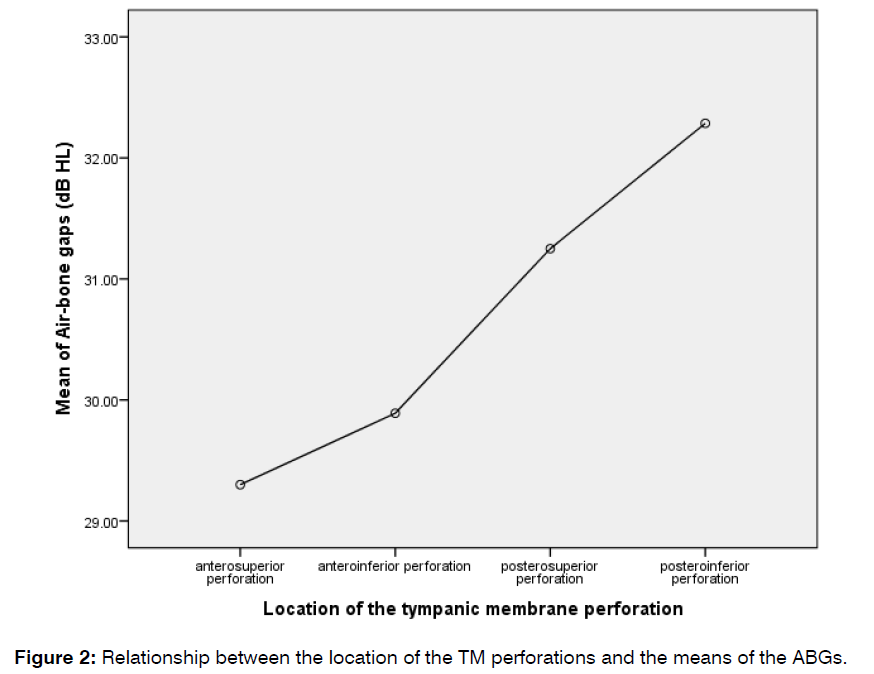
Figure 2: Relationship between the location of the TM perforations and the means of the ABGs.
The results of the Post Hoc Test (Scheffe test) for multiple comparisons among the different locations of TM perforations regarding the means of the ABGs were also not significant, as shown in Table 4.
| Location of the TM perforation | Air-bone gap's Mean Difference (dB HL) | Std. Error | P-value | |
|---|---|---|---|---|
| ASP | AIP | -0.571 | 1.583 | 0.988 |
| PIP | -2.986 | 1.673 | 0.371 | |
| PSP | -2.034 | 1.864 | 0.756 | |
| AIP | ASP | 0.571 | 1.583 | 0.988 |
| PIP | -2.415 | 1.230 | 0.287 | |
| PSP | -1.462 | 1.480 | 0.807 | |
| PSP | AIP | 1.462 | 1.480 | 0.807 |
| ASP | 2.034 | 1.864 | 0.756 | |
| PIP | -0.952 | 1.575 | 0.947 | |
| PIP | AIP | 2.415 | 1.230 | 0.287 |
| ASP | 2.986 | 1.673 | 0.371 | |
| PSP | 0.952 | 1.575 | 0.947 | |
Table 4: Post Hoc Test (Scheffe test).
Discussion
It is known that conductive hearing impairment is a consequence of TM perforations. However, there is still controversy regarding the relationship between the location of the TM perforation and the degree of conductive hearing loss.
In the current study, which was conducted on 74 patients with small TM perforations due to inactive mucosal CSOM, the most common location of the TM perforation was in the AI quadrant (40.54%), followed by the PI quadrant (31.08%), the PS quadrant (14.87%), and the AS quadrant (13.51%). Wicaksono et al., in their study of 43 patients with safe-type CSOM, found that the AI quadrant was the most common site of TM perforations (69.8%) [19]. Patel-Chudasama reported that the pars tensa, including the AI and PI quadrants, was the most common site of the TM perforations (81.4%) [20]. In another study conducted by Sood et al., they found that the most common location of the TM perforation was central (80%) [21].
The present study showed that the ABG’s means were 32.29 ± 5.41 dB HL, 31.34 ± 4.12 dB HL, 29.87 ± 3.48 dB HL, and 29.30 ± 4.60 dB HL in the PIP, PSP, AIP, and ASP, respectively. Although the ABG’s mean was greater in the PIP, statistical analysis showed that it was insignificant (P-value=0.168). Possibly, the greater hearing loss in the PIP, which was statistically insignificant, could be explained on the basis that the TM perforation in the PI quadrant leads to direct exposure of the round window, resulting in a sound pressure with the consequence of loss of the round window baffle, causing impaired cochlear response by a phase cancellation effect.
Virk et al., in their cross-sectional study that enrolled 246 patients with TM perforations due to inactive mucosal CSOM, mentioned that the PSP had 4–7 dB greater hearing loss than the ASP and AIP; however, it was statistically insignificant [22]. In a study conducted by Morris et al., and Saliba et al., they found no difference in hearing level between frequencies across all perforation sites [23, 24]. Pannu et al. stated that the hearing impairment was greater in posterior quadrant perforation than anterior quadrant perforation, but the difference was statistically insignificant (P-value<0.05) [11]. Similarly, the results of Mehta et al.,Vose et al., and Kumar et al.’s studies were in agreement with the results of the present study [13,25,26].
On the other hand, there are some studies that do not agree with the results of the current study. Khurshid et al. concluded that the degree of hearing loss was found to be directly affected by the location of the TM perforation, with the PSP producing the greatest degree of hearing loss [27], while Wicaksono et al. concluded that the PIP had a greater degree of conductive hearing impairment [19]. Similarly, Nahata et al. and Abdulsayed et al. concluded that the degree of conductive hearing loss is related to the location of the TM perforation [28, 29]. In a systematic review of 19 articles conducted by Basheer et al., the conclusion was that the anterior TM perforations cause less hearing impairment than the posterior, central, or marginal perforations [30].
However, ossicular coupling and acoustic coupling are the two pathways involved in sound transmission. Ossicular coupling is the main pathway for sound transmission in the normal middle ear; acoustic coupling (direct transmission of the sound energy to the oval and round windows) is less effective than ossicular coupling by about 60 dB, which makes it almost negligible in sound transmission in the healthy middle ear. In a perforated TM, there is an acoustic coupling gain of about 10–20 dB [31]. However, this acoustic coupling value is still much lower than the ossicular coupling value, so because of the insufficient acoustic coupling gain in patients with a small TM perforation, the degree of conductive hearing loss is not significantly affected by the location of the TM perforation [32].
Conclusion
In adult patients with small TM perforations due to inactive mucosal CSOM, the most common location of the TM perforation was the AI quadrant. Although the degree of conductive hearing loss was greater in the PIP, it was statistically insignificant. This study concluded that there was an insignificant correlation between the location of a small TM perforation and the degree of conductive hearing loss in adult patients with inactive mucosal CSOM.
References
- Kolo ES, Salisu AD, Yaro AM, Nwaorgu OG. Sensorineural hearing loss in patients with chronic suppurative otitis media. Electron Physician. 2012;64:59-62.
- Kumara A, Nigam R, Jain AK. Chronic suppurative otitis media: A clinicopathological study at a tertiary care hospital. IJAR. 2015;1(10):235-40.
- Rasheed AM, Taha YH. The Effect of Amoxicillin-Clavulanate and Actifed Versus Actived Only in treatment of Otitis Media with Effusion. J Faculty Med Baghdad. 2008;50(3):327-31.
- Rasheed AM. Adenoidectomy with Myringotomy and Tympanostomy Tube Versus Adenoidectomy with Myringotomy in Treatment of Otitis Media with Effusion in 5-7 Years Old Children. Al-Kindy College Med J. 2016;12(1):83-6.
- Afolabi OA, Salaudeen AG, Ologe FE, Nwabuisi C, Nwawolo CC. Pattern of bacterial isolates in the middle ear discharge of patients with chronic suppurative otitis media in a tertiary hospital in North central Nigeria. Afr Health Sci. 2012;12(3):362-7.
- Helmi. Chronic suppurative otitis media: basic knowledge of medical therapy tympanoplasty mastoidectomy. 2005.
- Park H, Hong SN, Kim HS, Han JJ, Chung J, Seo MW, et al. Determinants of conductive hearing loss in tympanic membrane perforation. Clin Exp Otorhinolaryngol. 2015;8(2):92-6.
- Rana AK, Upadhyay D, Yadav A, Prasad S. Correlation of tympanic membrane perforation with hearing loss and its parameters in chronic otitis media: an analytical study. Indian J Otolaryngol Head Neck Surg. 2020;72:187-93.
- Basheer HM, Rehman AU, Waseem H, Zaib W. Evaluating the causative factors that lead to rejection of hearing aids among young adults having moderate to severe degree sensorineural hearing loss. J Fatima Jinnah Med Univ. 2021;15(2):54-7.
- Clark JG. Uses and abuses of hearing loss classification. Asha. 1981;23(7):493-500.
- Pannu KK, Chadha S, Kumar D, Preeti. Evaluation of hearing loss in tympanic membrane perforation. Indian J Otolaryngol Head Neck Surg. 2011;63:208-13.
- Voss SE, Rosowski JJ, Merchant SN, Peake WT. How do tympanic-membrane perforations affect human middle-ear sound transmission? Acta Otolaryngol. 2001;121(2):169-73.
- Mehta RP, Rosowski JJ, Voss SE, O’Neil E, Merchant SN. Determinants of hearing loss in perforations of the tympanic membrane. Otol Neurotol. 2006;27(2):136.
- Gaur S, Sinha ON, Bhushan A, Batni G. Observations on tympanic membrane perforations (safe type) and hearing loss. Ind Otolaryngol Head & Neck Surg. 2017;69(1):29-34.
- Nepal A, Bhandary S, Mishra SC, Singh I, Kumar P. Assessment of quantitative hearing loss in relation to the morphology of central tympanic membrane perforations. Nepal Med Coll J. 2007;9(4):239-44.
- Ibekwe TS, Nwaorgu OG, Ijaduola TG. Correlating the site of tympanic membrane perforation with Hearing loss. BMC Ear Nose Throat Disord. 2009;9(1):1-4.
- Rasheed AM, Abbas AM, Hilal SA, Homadi NJ. Adenoidectomy and Endoscopic Myringotomy with and without ventilation tube insertion for Treatment of Otitis Media with Effusion in 6-12 years old Children. Int Tinnitus J. 2023;27(1):27-34.
- Rasheed AM. Is Topical Nasal steroid Useful for Treatment of Otitis Media with Effusion in Children? Int Tinnitus J. 2023;27(1):62-7.
- Wicaksono AB, Samodra E, Fitriana M, Trihandoko F, Khoiria AH, Dewanti DA. The Site Of Tympanic Membrane Perforation Influenced The Conductive Hearing Loss Level In Chronic Suppurative Otitis Media. J Med Sci. 2022;54(3).
- Meera PC. Correlating the severity of conductive hearing loss with the size and site of pars tensa tympanic membrane perforation using video-otoscopy Univ Nairobi Res Archive. 2012.
- Sood AS, Pal P, Kumar A. Tympanic membrane perforation: correlation of hearing loss with its site and size. Int J Otorhinolaryngol Head Neck Surg. 2018;4(2):397-402.
- Virk RS, Kudawla K, Bansal S, Rathod R, Behera S. Correlation of site and size of tympanic membrane perforation and middle ear air space volume with magnitude of hearing loss. Ann Otol Neurotol. 2019;2(01):10-5.
- Morris J, Lee Z, Sanchez L, Carney AS. Hearing loss increases with size but not site of tympanic membrane perforation in Aboriginal Australian children in remote locations. Laryngoscope Investig Otolaryngol. 2022;7(6):2050-6.
- Saliba I, Abela A, Arcand P. Tympanic membrane perforation: size, site and hearing evaluation. Int J Pediatr Otorhinolaryngol. 2011;75(4):527-31.
- Voss SE, Rosowski JJ, Merchant SN, Peake WT. Middle-ear function with tympanic-membrane perforations. I. Measurements and mechanisms. J Acoust Soc Am. 2001;110(3):1432-44.
- Kumar N, Chilke D, Puttewar MP. Clinical profile of tubotympanic CSOM and its management with special reference to site and size of tympanic membrane perforation, eustachian tube function and three flap tympanoplasty. Indian J Otolaryngol Head Neck Surg. 2012;64:5-12.
- Khurshid N, Khurshied S, Khizer MA, Hussain A, Safoor I, Jamal A, et al. Relationship of Hearing Loss and Tympanic Membrane Perforation Characteristics in Chronic Suppurative Otitis Media Patients. Cureus. 2022;14(12).
- Nahata V, Patil CY, Patil RK, Gattani G, Disawal A, Roy A. Tympanic membrane perforation: Its correlation with hearing loss and frequency affected-An analytical study. Ind J Otol. 2014;20(1):10-5.
- Atiyah RJ, Abdulsayed MN, Albbadri SA. Tympanic Membrane Perforations Site affect the Degree of Hearing Difficulty. Univ Thi-Qar J Med. 2018;16(2):163-71.
- Basheer HM, Ikram A, Hanif A. Degree of Hearing Loss in Association with Site of Tympanic Membrane Perforation: A Systematic Review. Pakistan J Med Health Sci. 2023;17(01):2-.
- Peake WT, Rosowski JJ, Lynch III TJ. Middle-ear transmission: acoustic versus ossicular coupling in cat and human. Hearing Res. 1992;57(2):245-68.
- Zakaria M, Othman N, Lih AC. Is the degree of hearing loss truly dependent on the site of tympanic membrane perforation?. Oman Med J. 2016;31(1):83.
Department of Surgery-Otolaryngology, College of Medicine, University of Baghdad, Baghdad, Iraq
Send correspondence to:
Ahmed Muhei Rasheed
Department of Surgery-Otolaryngology, College of Medicine, University of Baghdad, Baghdad, Iraq, E-mail: ahmed.muhei@comed.uobaghdad.edu.iq
Phone: 7713293222
Paper submitted on September 12, 2023; and Accepted on October 16, 2023
Citation: Rasheed AM. Does the Location of a Small Tympanic Membrane Perforation Affect the Degree of Hearing Loss in Adult Patients with Inactive Mucosal Chronic Suppurative Otitis Media?. Int Tinnitus J. 2023;27(2):135-140.


