The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 27, Issue 2 / December 2023
Research Article Pages:104-112
10.5935/0946-5448.20230017
Education Intervention on ′Hearing Impairment − Its Assessment and Management′ among Medical Practitioners in Sikkim, India
Authors: Anamika Sharma, Srividya A, Suresh T
PDF
Keywords: Awareness, Survey, Questionnaire, Sikkim, Medical professionals, Hearing loss, Cochlear implant.
Introduction
Hearing loss is the inability to hear as well as someone with normal hearing. Normal Hearing is, defined as having hearing thresholds of 20 dB or better in both ears. According to the world health organization (2021), the severity of hearing loss might range from slight to substantial. It makes it difficult to hear conversational dialogue or loud noises and can affect one or both ears. There are three main categories of hearing loss, each with a unique set of underlying causes, according to the American Speech- Language-Hearing Association (ASHA). Conductive hearing loss, Sensorineural Hearing Loss (SNHL), and mixed hearing loss are the three most typical causes of diminished hearing [1].
The most prevalent sensory deficiency is hearing loss, which affects 1 in 1000 newborns and can range from mild to profound [2]. This study also reports that the number may raise to 17 in 1000 by age 18 and this rise can be attributable to a variety of factors, including progressive, acquired, or late-onset inherited reasons. Early diagnosis of hearing loss is important to reduce the negative effects on the health and quality of life of the affected kid and his or her family [1]. According to the world health organization (2022) recently, more than 1.5 billion people (nearly 20% of the global population) live with hearing loss. 430 million of them have disabling hearing loss.
The most prevalent sensory deficiency is hearing loss, which affects 1 in 1000 newborns and can range from mild to profound [2]. This study also reports that the number may raise to 17 in 1000 by age 18 and this rise can be attributable to a variety of factors, including progressive, acquired, or late-onset inherited reasons. Early diagnosis of hearing loss is important to reduce the negative effects on the health and quality of life of the affected kid and his or her family.
State of Sikkim has around 1489 registered medical practitioners, of which 150 are ENT specialists registered at AOL and 03 is no of audiologists for a population of 683000 according to census data 2021.. Though medical seminars and workshops are common, topics related to audiology, hearing impairment, CI, are rare.
According to the World health organization (2012), around 5.3% (or 360 million people) of people worldwide have hearing loss. Children make up 9% of those. Hearing loss of 61 dBHL or more in the better ear is deemed to be severe to profound hearing loss [3]. The prevalence is reported to be 6.3% of population in India (NSSO, 2001). Children in age range of 1-14yrs are the majority. Studies give different figures of incidence. Prevalence of 6% and 26.9% is reported by community based studies. Hearing losses that are in range of disability is reported to be between 4.5% and 18.3% [4]. Hearing loss prevalence and severity are known to vary depending on several factors, such as socioeconomic status, exposure to diseases, and consanguinity [5]. Hearing loss is more prevalent as people get older and have less money [5]. In order to identify potential prevalence of hearing impairment in Sikkim and plan for increased services, there is requirement of support of medical practitioners. They can help in identification and proper referral.
The present study aimed at assessing medical practitioner of Sikkim’s knowledge about hearing impairment, diagnosis and management of it, audiological services, before and after an educational intervention, by way of a 2-hour lecture focused on hearing impairment and current status of its management.
This professional population was important for the study as,
a) There is a need for increased audiological services in the region to reduce burden of likely undiagnosed hearing loss in school-aged children in the region.
b) The significant challenges in identifying these individuals.
Aim of the Study: To evaluate impact of education intervention (awareness program) on knowledge of medical practitioners about hearing impairment, in the state of Sikkim India.
Objective of the Study: To evaluate knowledge about hearing impairment, its assessment and management among medical practitioners in Sikkim by using the pre survey questionnaire before the education intervention awareness program.
To evaluate knowledge about hearing impairment, its assessment and management among medical practitioners in Sikkim by using the post survey questionnaire after the education intervention awareness program. To evaluate change in level of knowledge about hearing impairment, its assessment and management among medical practitioners in Sikkim by pre survey and post survey comparison.
Need of the Study: The Indian state of Sikkim is situated in the eastern Himalayas in the northeastern region of the nation. It is one of the tiniest states in India. 6.79 Lakh people make up Sikkim’s current population. In the state of Sikkim, there are no speech and hearing institutes. In the State, which has a population of 6.79 lakh, there are only six SLPs and Audiologists.
Medical practitioners are usually the first point of contact by the general public for any condition to a hearing issue. Majority of them in Sikkim do not have opportunities to attend any workshops or seminars on hearing loss or early intervention.
The purpose of this study was to compare the effectiveness of an awareness presentation before and after completing an awareness program regarding hearing impairment, its assessment, and management in the State of Sikkim.
Medical practitioners are the primary referral for audiologists. They also help in installing confidence among ordinary public about clinical services offered by audiologists and also may also ensure patients seek audiological services without delay. Therefore it’s important that medical practitioners have current information about hearing loss, its management and understand the complexities involved in it. Management of hearing loss, tinnitus and vertigo often requires multidisciplinary approach. It has been realized that a single expert cannot completely meet each patient’s needs while taking the patient’s welfare into consideration, hence interdisciplinary collaboration is required6. Complications can arise when professionals are not fully aware of the obligations of the other profession [7]. This affects the kind and frequency of recommendations.
Hence need for an awareness program targeting medical professionals was felt.
Method
Data was collected in city of Sikkim by primary investigator and later analyzed by co investigators at the Dr SRCISH. All the Major Hospitals and medical colleges were visited and information about the education intervention awareness program and the study was spread. This was done in order to have diverse representation of medical practitioners in the sample of the study. It was part of Dissertation work of primary investigator. Approval of the scientific committee and Institutional Ethical Committee were obtained by following due process.
Research Design: A non-experimental, pre survey -post Survey comparison research design was used for the purpose of this research.
Sample Size: According to a study titled “Sample Size Estimation Using Yamane and Cochran and Krejcie and Morgan and Green Formulas and Cohen Statistical Power Analysis by G*Power and Comparisons,” we can use 15% to 30% of the population as sample size if there are hundreds of persons in the population [8]. The registered number of medical practitioners in state of Sikkim according to Indian Medical council is 1489. Therefore 15% of 1489 or 225 practitioners were sent invitations to participate in the study.
Participants: The study participants were selected based on the following inclusion – exclusion criteria.
Inclusion Criteria
• Medical practitioners belonging to any medical specialty were included (General physicians, Otolaryngologist, Dentist, Dental Surgeon, General Surgeon, Oncologist, Cardiologist, Psychiatrist, Neurologist, Radiologist, Pulmonologist, Gastroenterologist, Microbiologist and Pediatricians).
• Should be practicing in State of Sikkim for longer than 6 months at the time of the study.
• Should consent to attend awareness program conducted by the researcher.
Exclusion Criteria
• Medical practitioners who were outside the State of Sikkim at the time of the study
• Who were unwilling or could not attend both pre and post-survey.
• Who had any family member or friend or self with a hearing, speech, or language disorder (To exclude participants who already have some knowledge).
• Who had any family member who is a hearing, speech, or language specialist (To exclude participants who already have some knowledge).
• Medical practitioners belonging to alternative medicine like ayurveda, unani and homeopathy.
Overall, 48 subjects were included in the current investigation.
Data Collection Tool: The present study was designed to collect the responses of participants using questionnaire. The questionnaire tool was developed for the purpose of the study and content validated. In order to address the objectives of the study, items belonging to three domains were chosen. They were related to hearing impairment, assessment of hearing impairment and to management of hearing impairment. The steps in the development of questionnaire tool are given below
Step1: To develop a questionnaire to measure awareness about hearing impairment- It’s assessment and management.
The items of the questionnaire for Medical practitioners were organized into four sections namely: The demographic data, sections on hearing impairment, section on assessment, and section on the management.
Part 1: General demographic data of the participants. This section will have six questions, which include: name, age, gender, E-mail id, and speciality, duration of working experience.
This section will have six questions, which include: name, age, gender, E-mail id, and speciality, duration of working experience.
Part 2: Knowledge about hearing impairment and its causes.
This section consisted of questions about hearing impairment and its causes, which will evaluate the respondent’s knowledge about hearing impairment and its cause.
Part 3: Knowledge about assessment of hearing impairment among medical practitioners in Sikkim.
This section consisted of about the assessment of hearing impairment, which will evaluate the respondent’s knowledge about the assessment of hearing impairment.
Part 4: Knowledge about management of hearing impairment among medical practitioners in Sikkim.
All the questions were statements. Respondents had to choose an option on 5 point rating scale, varying from strongly disagree to strongly agree.
Content Validation: The questionnaire was subjected to content validation. It was given to five faculties with 5-8years of experience in the field of audiology and to five medical practitioners. They were asked to rate the questions/ items on a likert’s 5 point scale, for the appropriateness of questions for the stated objectives. The questions/items which were rated as most appropriate or appropriate were included in the final questionnaire.
Following content validation process, five questions for section II, nine questions for section III and 11 questions for section IV were retained. The questionnaire was made as a hard copy and provided for the administration of medical practitioners in the state of Sikkim.
Step 2: Development of material for education intervention, awareness event.
A Microsoft PowerPoint was made with the information regarding hearing loss, its causes and types, early identification and early intervention, obstacles of early identification, benefits of early identification and intervention, tests for screening children with hearing loss, benefits of early detection of hearing loss and its benefits, treatment for children, adults and geriatrics with hearing loss, need of hearing aids and cochlear implant, auditory training, the role of the audiologist in hearing loss management, management and treatment options available, prevention and education, the team of professionals involved, audiological test battery, and ways to prevent hearing loss.
Content validation was done for the content of the slides used in relevance to the questionnaire and also the objective of the study. The material for the PowerPoint presentation was prepared and subjected to validation. The five audiologists rated the slides for content, relevance, clarity and accuracy of the information on a five point likert’s scale.
Procedure of the Study: The researcher contacted medical practitioners of different hospital set ups over telephonic conversation and in person visit. Permission from the hospital board was obtained before initiating the study. The participants were informed about the scope, procedure, and details of the study, and consent to participate were taken before collecting data from them. The participants were requested to attend an education intervention event, a talk arranged in the seminar hall of a medical college. The participants were asked to fill in the pre-questionnaire, before the talk and the responded were given the fresh set of questionnaire again to fill it in, post attendance of awareness event. The collected responses (both pre and post-survey) from the participants were analyzed questionnaire was collected by the researcher. A talk with the help of Power Point presentation was given by the researcher. The content included information on Hearing impairment its assessment and management. This was to create awareness among the participants.
Statistical Analysis: All the data obtained were tabulated using Microsoft Office Excel. Data was subjected to descriptive statistics analysis using SPSS 20 (version 20.0) software. The data was categorical in nature. Results of the Knowledge Surveys were analyzed by calculating the percentage of agreement and disagreement. The percent agreement included responses for “Strongly Agree” and “Agree” while percent disagreement included responses for “Strongly Disagree” and “Disagree”.
Improvement in knowledge post education intervention was measured by calculating percentage difference of disagreement and agreement between pre and post survey questionnaire. The percent increase was calculated by dividing the difference in Pre- and Post-Survey scores by the Pre-Survey score. The non-parametric test, chi-square test was used to check whether there is any significant change in the level of awareness about hearing impairment its assessment, and management among medical practitioners in Sikkim after conducting the awareness program.
Results
The aim of the present study was to determine the knowledge level about ‘hearing impairment – its assessment and management among medical practitioners in the state of Sikkim, India and to mark the change in awareness level after attending a talk on hearing impairment. Results were computed and given in sections below.
Descriptive Statistics
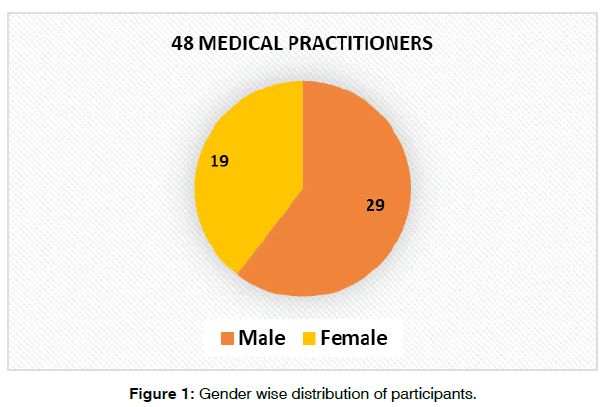
Section I- Demographic Information: In congruence with population characteristics, the gender ratio of the sample of our study also reflected predominant male gender; female n=19: Male n=29. (Figure 1).
There were 10 participants in the age range 25-35 yrs, 18 participants each in the age range 36-45yrs and 46-55yrs and 2 participants in the age range 55-65yrs.
a) Work experience: Work experience ranged 1- 40 years.
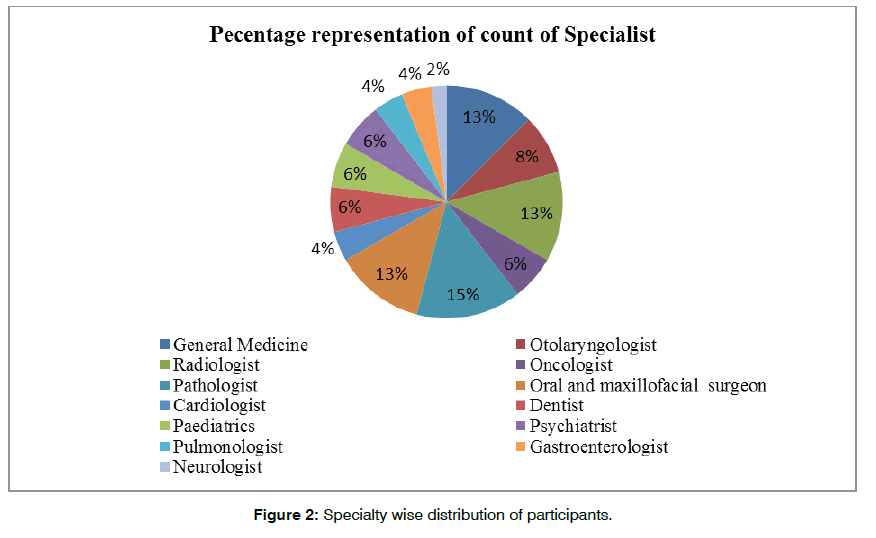
b) Specialty (Figure 2).
The results show that there was representation from many specialties and proportion of representation of each discipline was similar. Least representation was seen for neurology (one subject) and cardiology (two subjects).
Section II: Hearing Impairment: The overall agreement for questions statements among subjects ranged from 70.83% (Q2) to 95.8% (Q1) at pre survey i.e. before education intervention. At post education intervention percentage agreement reached 100% among subjects as expected. Only Q3 received 97% i.e one subject answered by choosing disagree option for it (Table 1). Knowledge about Nature of hearing impairment, its causes as expected was adequate among medical practitioners. But association of hearing impairment to handicap, speech language delay and progressivity were poor among them before education intervention. The awareness talk helped them to acquire these information as well.
| Q | Section II- Hearing Impairment | Pre survey-Agreement (% of respondents) |
Post Survey Agreement (% of respondents) |
|---|---|---|---|
| Q1 | Hearing loss refers to the total or partial inability to hear sounds | 95.833 | 100 |
| Q2 | Hearing loss is a condition that can be extremely handicapping | 70.833 | 100 |
| Q3 | Hearing loss can be sudden or progressive impairment. | 81.250 | 97.91 |
| Q4 | Hearing loss can cause a delay in speech and language development in children. | 87.500 | 100 |
| Q5 | Hearing loss gets worse over time and affects all age groups. | 72.917 | 100 |
| Q6 | Hearing loss is associated with ruptured eardrum, excessive noise exposure, and physical trauma. | 91.667 | 100 |
Table 1: Scores of agreement for Section II- Hearing Impairment.
Section III: Assessment: Results show that information about assessment procedures and its application is lacking among medical practitioners. Pre Survey results showed that percentage agreement to question statements in section II were low. Q7 about behavioral observation audiometry received least score of 34% which improved to 75% post survey. Q11 and Q12 about pure tone audiometry and admittance respectively had received only around 50% scores at pre survey, while both questions showed 100% scores post survey (Table 2).
| Q | Section III- Assessment | Pre survey Agreement (% of respondents) |
Post Survey Agreement (% of respondents) |
|---|---|---|---|
| Q7 | Behavioral observation audiometry and condition play audiometry is used to test infants and pre-schoolers. | 34.23 | 75.00 |
| Q9 | Children with hearing loss develop language at a slower rate than normal-hearing peers. | 85.42 | 100.00 |
| Q10 | Pure tone audiometry measures the degree and type of hearing loss. | 77.08 | 100.00 |
| Q11 | Pure tone audiometry uses frequency-specific tones for testing. | 58.33 | 100.00 |
| Q12 | In addition to examining the middle ear status, admittance also helps us understand cranial nerve VII and VIII functioning. | 50.00 | 100.00 |
| Q14 | Medical history, laboratory tests, and physical examination are mandatory before cochlear implant surgery. | 85.42 | 100.00 |
| Q15 | Psychological evaluation is mandatory before cochlear implantation. | 75.00 | 100.00 |
| Q16 | Early identification, diagnosis, and treatment of mild-to-moderate hearing loss prevent further deterioration of hearing. | 83.33 | 97.91 |
Table 2: Scores of agreement for Section III- Assessment.
Q8 about hearing screening is a negatively scored question, with agreement reflecting lack of knowledge about hearing screening and disagreement being vice-versa. Results of this important question on importance of hearing screening showed that only 34% were aware of correct role of hearing screening at pre survey. Knowledge about this improved significantly post survey, to 75%, but not reaching 100%.
Section IV: Management: Table 3 shows that medical practitioners were not well informed about management aspects of hearing impairment. Pre survey agreement for all question statements ranged from 58.33% (Q23) to 89.58% (Q18). Question related to auditory processing received the least score agreement i.e 58.33%. Post survey scores were all seen to be reaching 95% to 100%.
| Q | Section III- Management | Pre Survey Agreement (% of respondents) |
Post Survey Agreement (%of respondents) |
|---|---|---|---|
| Q17 | Medical treatment alone is enough for treating hearing loss. | 25.0% | 10.4% |
| Q18 | Sudden hearing loss is an emergency and require and immediate audiological assessment. | 89.5% | 95.8% |
| Q19 | Cochlear implant/hearing aid restores hearing. | 64.5% | 31.2% |
| Q20 | Hearing loss seen in the aging population can be preventable. | 41.6% | 89.6% |
| Q21 | Hearing aids are primarily useful in improving the hearing and speech comprehension of people with hearing loss. | 87.5% | 100% |
| Q23 | Audiologist evaluates and manages children and adults with central auditory processing disorders. | 58.3% | 100% |
| Q25 | Assistive listening devices are useful for children with hearing loss. | 75.0% | 100% |
Table 3: Scores of agreement for Section IV- Management.
Comparison of Scores on Pre and Post Awareness Responses to Questionnaire: To measure the change in awareness after education intervention, as indicated by scores of agreement for Section II, III and IV, among medical practitioners, the non-parametric test, chi square test was applied. This test will compare the level of awareness among the medical practitioners, before and after the awareness program (Table 4).
| Q | No. of Participants |
Pre Survey Count of Responses (Agreement) |
Pre Survey Count of Responses ( Agreement) |
X2 | Pre-Post (p-value) |
|---|---|---|---|---|---|
| Q1 | 48 | 46 | 0.36 | 0.545 | |
| Q2 | 48 | 34 | 13.35 | 0.0002 | |
| Q3 | 48 | 39 | 7.14 | 007 | |
| Q4 | 48 | 42 | 3.96 | 0.045 | |
| Q5 | 48 | 35 | 12.31 | 0.00045 | |
| Q6 | 48 | 44 | 1.96 | 0.1611 | |
| Q7 | 48 | 32 | 47 | 17.50 | 0.00002 |
| Q8 | 48 | 31 | 12 | 17.50 | 0.00002 |
| Q9 | 48 | 41 | 47 | 4.09 | 0.043 |
| Q10 | 48 | 37 | 48 | 8.54 | 0.0034 |
| Q11 | 48 | 28 | 48 | 21.0 | 0.0001 |
| Q12 | 48 | 24 | 48 | 29.59 | 0.00001 |
| Q13 | 48 | 37 | 48 | 12.31 | 0.00045 |
| Q14 | 48 | 41 | 48 | 4.90 | 0.046716 |
| Q15 | 48 | 36 | 47 | 12.31 | 0.00045 |
| Q16 | 48 | 40 | 05 | 6.00 | 0.014 |
| Q17 | 48 | 12 | 46 | 6.00 | 0.000 |
| Q18 | 48 | 43 | 46 | 2.84 | 0.0916 |
| Q19 | 48 | 31 | 15 | 8.54 | 0.0034 |
| Q20 | 48 | 20 | 43 | 24.42 | 0.0001 |
| Q21 | 48 | 42 | 48 | 2.84 | 0.0916 |
| Q22 | 48 | 22 | 02 | 17.50 | 0.000 |
| Q23 | 48 | 28 | 48 | 22.98 | 0.000 |
| Q24 | 48 | 22 | 02 | 13.35 | 0.000 |
| Q25 | 48 | 36 | 48 | 12.31 | 0.00045 |
Table 4: Chi-square and p values for pre & post comparison (item wise).
Results of chi square test are also tabulated in table 4 (x2 and p value). It suggests that except for Q1, 18and 21 all other questions, null hypothesis is to be rejected. The difference in median values of choices of responses differed significantly between pre and post awareness talk. The awareness talk did have significant effect on knowledge of medical practitioners about hearing impairment, assessment and management of it.
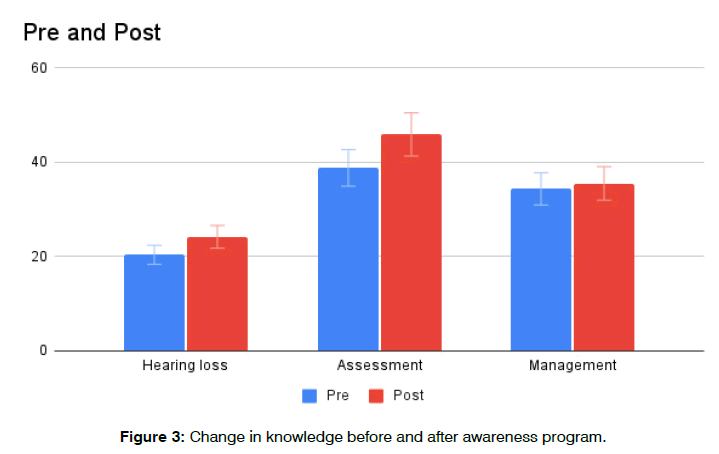
Test Retest Reliability Analysis: Questionnaire was re administered on 10% of the subjects after a 3 month postawareness program to assess whether they retain the knowledge learnt due to awareness program. The obtained coefficient correlation factor was 0.92. Therefore it was concluded that the responses showed good agreement when administered at post awareness program and at 3 months period after awareness program (Figure 3).
Discussion
The study consisted on custom questionnaire development and validation and administering on group of medical practitioners. The questionnaire was validated by five audiologists and medical practitioners and agreed upon that items test the objectives of the study well. Content of awareness program was also validated by five audiologists. This validated tool was administered on 48 respondents before awareness program was initiated and soon after awareness program was conducted.
The results of the study, demonstrates adequately, medical practitioners are lacking in their knowledge of assessment and management of hearing impairment and they benefitted from education intervention offered through the course. Table 4 clearly demonstrates that medical practitioner’s answers to items improved post awareness. Other studies have also demonstrated that education interventions are effective in improving knowledge about hearing impairment among key stake holders. A study reported an increase from 55% scores to 68% scores on health literacy among community health workers after they attended a training program [9]. One another similar study reported knowledge of teachers improved to almost 97% scores after attending an education intervention program [10].
The responses showed the knowledge among medical practitioners at pre awareness survey, for section I, about hearing impairment was adequate with majority choosing ‘agree’ or ‘strongly agree’ as responses. Whereas items in section II and III, assessment and management showed responses to be distributed among choices of ‘don’t know’ ‘disagree’ along with ‘agree’ at pre awareness survey. There was significant number of items for which respondents didn’t choose the right option. This demonstrates while medical practitioners may be broadly aware of hearing impairment and its management , they may not be aware of specific information like tests done, its usage, impact of management etc. Many weren’t aware that pure tone testing involved testing at specific frequencies (Q11) or that immittance testing would help in cranial nerve VIII and VII assessment (Q12). In management section, only 12 respondents chose agree option for question ‘medical treatment alone is enough for treating hearing loss’ at pre awareness survey and it reduced to 5 respondents at post awareness survey. Large no of respondents therefore (75%) are aware that hearing impaired individuals would require hearing aids, CI etc, not medical treatment alone. Almost 80% of respondents were not aware of Audiologists role in auditory processing at pre awareness survey (Q25 Table 4) which implies majority are still not aware of all the aspects of responsibility and skills of audiologists.
Hearing health services are required at any part of India. Specially there is a growing number of elderly population and hearing loss is prevalent among that age group. Children are prone to middle ear disorders which are treatable and hearing loss in them therefore preventable. Awareness among all stakeholders therefore becomes essential in order to achieve hearing health for all, a target set by WHO (2022). Hearing health is also SDG 2 and early intervention can help reduce burden to individual and society due to disability. All these have impact on govt policies related to SDG. Therefore there should be an ongoing effort at organizing education programs to stakeholders like, medical practitioners, health workers, teachers at different part of the country. Remote places probably require such assistance more than elsewhere.
Conclusion
• Medical practitioners from various specialties like, General physicians, pediatricians, radiologists, pulmonologists, gastroenterologists, neurologists, cardiologists, dental surgeons, dentists, and otolaryngologists working in Sikkim took part in this study.
• Lack of knowledge regarding assessment and management aspects of hearing impairment were evident at pre awareness survey.
• Post awareness responses to questionnaire showed impact of awareness program.
• Responses were 100% or closer to 100% correct response at post awareness survey
• The sample included all specialties of medical practitioners in Sikkim.
Future Recommendations
• More of such awareness programs can be conducted among the medical practitioners / general public / schools and primary health centers.
• Size of participants were less, probably more effort to be put in to generate interest among medical practitioners on attending hearing health related seminars.
• Educating healthcare professionals about the role of corresponding experts and promoting consultation within the group and acknowledge the need of audiologist at the right time.
References
- Moeller MP, White KR, Shisler L. Primary care physicians' knowledge, attitudes, and practices related to newborn hearing screening. Pediatr. 2006;118(4):1357-70.
- Grindle CR. Pediatric Hearing Loss. Pediatr Rev. 2014;35(11):456–464.
- Mathers C, Smith A, Concha M. Global burden of hearing loss in the year 2000. Global Burden Dis. 2000;18(4):1-30.
- Verma RR, Konkimalla A, Thakar A, Sikka K, Singh AC, Khanna T. Prevalence of hearing loss in India. Natl Med J India. 2021;34(4).
- Stevens G, Flaxman S, Brunskill E, Mascarenhas M, Mathers CD, Finucane M. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. Eur J Public Health. 2013;23(1):146-52.
- Green BN, Johnson CD. Interprofessional collaboration in research, education, and clinical practice: working together for a better future. J Chiropr Educ. 2015;29(1):1-0.
- Björklund K, Silén C. Occupational therapy and physiotherapy students’ communicative and collaborative learning in an interprofessional virtual setting. Scand J Occup Ther. 2021;28(4):264-73.
- Chaokromthong K, Sintao N. Sample size estimation using Yamane and Cochran and Krejcie and Morgan and green formulas and Cohen statistical power analysis by G* Power and comparisions. Apheit Int J. 2021;10(2):76-86.
- Mulwafu W, Ensink R, Kuper H, Fagan J. Survey of ENT services in sub-Saharan Africa: little progress between 2009 and 2015. Glob Health Action. 2017;10(1):1289736.
- Kapalamula G, Gordie K, Khomera M, Porterfield JZ, Toman J, Vallario J. Hearing Health Awareness and the Need for Educational Outreach Amongst Teachers in Malawi. Audiol Res. 2023;13(2):271-84.
Assistant Professor, Bangalore Speech and Hearing Research Foundation, Chandrasekhar institute of Speech and Hearing, Bangalore, India
Send correspondence to:
Srividya A
Assistant Professor, Bangalore Speech and Hearing Research Foundation, Chandrasekhar institute of Speech and Hearing, Bangalore, India, Email: the.srividya@gmail.com
Tel: 9880938138
Paper submitted on July 12, 2023; and Accepted on July 20, 2023
Citation: Sharma A, Srividya A, Suresh T. Education Intervention on ‘Hearing Impairment – Its Assessment and Management’ among Medical Practitioners in Sikkim, India. Int Tinnitus J. 2023;27(2):104-112.