The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 21, Issue 2 / December 2017
Research Paper Pages:98-103
Effects of Smoking on Eustachian Tube and Hearing
Authors: Matteo Pezzoli, Denise Lofaro, Alessandro Oliva, Monica Orione, Daniela Cupi, Andrea Albera, Guido Bongioannini, Roberto Albera
PDF
Abstract
Objective: The purpose of this study was to evaluate the effect of tobacco use on the Eustachian tube and inner ear function. Study Design: Case-control study. Subjects and settings: Thirty-one nonsmoking volunteers and 34 smoking subjects recruited in an University Hospital, submitted to an audiological evaluation including pure tone audiometry, basal tympanogram, stapedial reflexes analysis, and nine-step eustachian tube (ET) function test. Results: Pure Tone Average (PTA) threshold at all frequencies tested was 12.5 dB in smokers and 3.7 in nonsmoking subjects. Nine smokers (27%) presented some degree of hearing loss versus none in the nonsmoker group. Linear regression analysis showed a higher degree of sensorineural hearing loss with age in smokers. Among the smokers, 20 subjects (59%) presented an impaired tubal function for the nine-step inflation/deflation tympanometric test, while only 6 (19%) subjects in the group of nonsmokers showed a tubal dysfunction. Conclusion: Tobacco use may reduce the ability to hear, mainly causing a sensorineural hearing loss for higher frequencies. We also found the presence of a high number of smokers suffering from tubal dysfunction. This has an important clinical relevance, not only because smoking increases the incidence of middle ear diseases, but also because tubal dysfunction may cause nonspecific symptoms characterised by ear fullness and difficulties in middle ear equalisation.
Keywords: smoke, tobacco, eustachian tube, hearing loss
Introduction
According to the World Health Organization, smoking is the leading easily avoidable cause of death, responsible each year for the death of approximately 5 million people around the world due to cancer, cardiovascular disease, and respiratory disease [1].
Smokers all over the world number approximately 650 million people, while in Italy, according to recent available data, the number of smokers is around 11 million people, equivalent to 21.7% of the Italian population over 14 years of age [1]. Despite the improvements in public health due to tobacco control policies, the harmful impact of tobacco smoke remains a major problem.
Focusing on the auditory system, smoking and passive smoke exposure may be associated with the onset of middle and inner ear pathologies, due to the harmful effects of smoke constituents such as carbon monoxide, tar, and nicotine [2]. However, even if the adverse effects of cigarette smoking on hearing loss have been demonstrated in previous population-based studies [3,4], other studies have not confirmed such an association [5,6]. It has been postulated that passive smoking may be a risk factor for development of minimal hearing loss also in the paediatric population [7].
Tobacco smoking seems to affect the inner ear through several mechanisms that can be categorized as direct or indirect. Toxic cigarette substances induce direct oxidative damage mediated by reactive oxygen species (ROS) and free radicals that are capable of damaging many cellular components such as DNA, protein and lipids [8], leading to neurosensory hearing loss that affects especially higher frequencies. Indirect damage is mediated by the vasospastic effect caused by nicotine, by the acceleration of atherosclerosis in the vascular loops of the auditory system [9] and by the increased levels of carboxyhaemoglobin and increased blood viscosity. All these factors reduce oxygen perfusion in the organ of Corti [10]. Moreover, smoking can act as a risk factor for noise-induced hearing loss since smokers simultaneously exposed to noise in the workplace were affected by a higher degree of hearing loss than nonsmokers [4,11,12].
With regard to harmful effects of smoking on middle ear, previous studies were conducted in the paediatric population, to investigate if otitis media, due to a eustachian tube dysfunction (ETD), was related to cigarette smoking. Even if a review of the literature conducted in 1995 did not find adequate evidence of the association of passive smoking and ETD [13], more recent studies show that children who are exposed to second-hand smoke have an increased risk of developing chronic otitis media with effusion [14]. Tobacco-specific nitrosamines, a group of carcinogens produced by nicotine and tobacco-derived alkaloids, in fact, can determine squamous metaplasia of the tubal mucosa and depletion of its hair cells, delegated to the mucociliary function of the eustachian tube. The loss of mucociliary clearance mechanisms,allergic response of the mucosa to substances contained in the tobacco smoke, chemical irritation and overall immunosuppressive effects secondary to tobacco smoke exposure could lead to greater susceptibility to bacterial infections of the middle ear [15].
Gaur found in a retrospective study that middle ear diseases were significantly more common in smokers [2]. Sharabi et al. showed that conductive hearing loss was more common than sensorineural hearing loss in current and past smokers [16]. Patel et al. found, in a large cohort of paediatric patients a mild association between passive smoking and ETD [15]. However, data on the effects of tobacco in the pathogenesis of diseases of the middle ear in the adult population are scarce, to date, and there exist no studies in the literature aimed at the analysis of its effect on the tubal function in its entirety.
The purpose of our study is to evaluate tubal function and hearing threshold in an adult population of smokers, in order to confirm the association of sensorineural hearing loss and to study the effect of tobacco on the eustachian tube.
Materials and Methods
The sample was composed of 34 smokers, recruited from consecutively referred patients to our hospital-based tobacco clinic and 31 non-smoking volunteers recruited from the hospital staff and their relatives. The study protocol was approved by the Ethical Committee of Mauriziano Hospital, Torino. The study group was composed only of subjects who had smoked five or more cigarettes a day for over a year with a normal baseline tympanogram (peak compliance between +50 and -100 mm/H2O) and with a normal stapedial reflex. All subjects submitted to an ENT examination, were asked to complete a questionnaire about their medical history, smoking habits, risk factors for noise-induced hearing loss (chronic noise exposure during work/ leisure, use of firearms) and were asked if they were suffering from cold or sinus problem. Hypertension was identified if the participant reported that they had hypertension or currently took medication for high blood pressure. Subjects suffering from chronic middle ear pathologies, chronic rhinitis, hypercholesterolemia, diabetes, previous head trauma or occupational exposure to noise were excluded from the study. Also, subjects affected by acute upper way at the time of the test pathologies were excluded from the study. The mean age of subjects from the study group was 42.6 years (standard deviation (SD), 12.6 years; range, 25-65 years); 14(41%) were males and 20(59%) were females.
Thirty-one healthy subjects gave informed consent and were enrolled as controls, applying the same exclusion criteria of the study group. The mean age of subjects from the control group was 40.6 years (SD, 13.1 years; range 20-59); 15(48%) were males and 16(52%) were females. Differences in sex distribution and age between smokers and non-smokers were not significant according to the chi square test and Student’s t test (p > 0.05), respectively. For each smoker, the level of exposure to cigarettes was also calculated, expressed as “Pack Year” (number of packs of cigarettes smoked per day for years of exposure). All of the subjects, smokers and nonsmokers, were submitted to an audiological evaluation including pure tone audiometry, with data recorded for the hearing threshold, basal tympanogram, stapedial reflexes analysis, and nine-step eustachian tube function test. Hearing test was always carried out in a soundproof chamber at least 16 hours after the last significant noise exposure (attending nightclubs or live music events). The frequencies evaluated, for both ears, were 250, 500, 1000, 2000, 4000, 6000, and 8000 Hz.
The nine-step inflation/deflation tympanometric test developed by Bluestone [17] was carried out according to the following steps. The test begins with a baseline tympanogram to establish a reference value (first step); then the ear canal pressure was increased to +200 mm/ H2O so that the tympanic membrane moves toward middle ear. At this point patients were asked to swallow three times to equilibrate middle ear overpressure via the eustachian tube (second step). If the equilibration was successful, the second tympanogram documented the established middle ear underpressure (peak at a negative pressure - third step). After the audiologist normalizes the ear canal pressure subjects again swallowed three times to equilibrate negative middle ear pressure that was provoked during the first three steps. (Fourth step) Then, the tympanogram was repeated in order to measure middle pressure after re-equilibration (the peak returns toward 0 daPa- fifth step). The same procedure was performed with -200 mm/H2O ear canal pressure between (sixth to ninth steps); in this case, the expected pressure changes were towards positive values.
Failure to alter middle ear pressure at least 10 mm/H2O with swallowing during any of the third, fifth, seventh, or ninth steps was considered to be due to a eustachian tube dysfunction, whereas if the equilibration was successful in all steps, eustachian tube function was considered normal. We did not differentiated between poor eustachian function and no function at all.
All statistical analyses were conducted using the Graph Pad Prism 5 package (Graph Pad Software Inc., La Jolla, California, USA). Chi-square analysis was used to investigate qualitative variables (number of subjects with hearing loss on high frequencies and tubal dysfunction); T-test was performed to compare the average of the hearing deficit between the two groups concerned, whereas linear regression analysis was performed to assess how the hearing deficiency varies with increasing cigarette consumption, age and hypertension. Binary logistic regression analysis, taking PTA as dependent variable, and smoking habit and age as independent variables, was performed to determine the effect of smoking on hearing threshold variance. This study was conducted in accordance with the Declaration of Helsinki.
Results
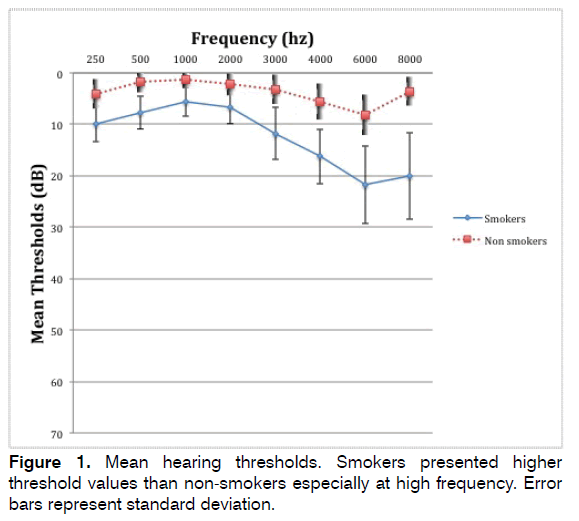
PTA at all frequencies tested (250-8000) was 12.5 dB (SD = 7.1) in smokers and 3.7 (SD = 2.8) in nonsmoking subjects; the difference was significant according to the Student’s t test (p < 0.0001), as reported in Table 1. Figure 1 reports the mean audiogram in smokers and in non-smokers; smokers presented higher threshold values.
| Smokers | Non smokers | P-Value | |
|---|---|---|---|
| No. | 34 | 31 | |
| Males (%) | 14 (41%) | 15 (48%) | > 0.05 |
| Mean age (SD) | 42.6 (12,6) | 40.6 (13.1) | > 0.05 |
| PTAa 250-8000 (SD) | 12.5 (7.1) dB | 3.7 (2.8) dB | < 0.0001 |
| HF Hearing loss (%) | 9 (27%) | 0 | < 0.01 |
| Hypertension | 7 (21%) | 1 (3%) | > 0.05 |
| Poor Eustachian function (%) | 20 (58%) | 6(19%) | < 0.05 |
PTAa: Pure Tone Average.
Table 1. Characteristics of subjects admitted in the study group and classified as smokers and non-smokers. Smokers presented a significantly higher mean PTA threshold, a significantly higher number of subjects with HF hearing loss and a significantly poorer Eustachian tube function.
Since hearing loss was always sensory-neural and limited to the higher frequencies, we have also evaluated mean PTA values at 3000, 4000, 6000, and 8000 Hz (HF hearing loss) and, according to literature, we have considered pathological threshold values more than 25 dB at the worse ear. Nine smokers (27%) presented some degree of hearing loss versus none in the non-smoker group (p = 0.006, chi squared equals 7.43 with 1 degrees of freedom).
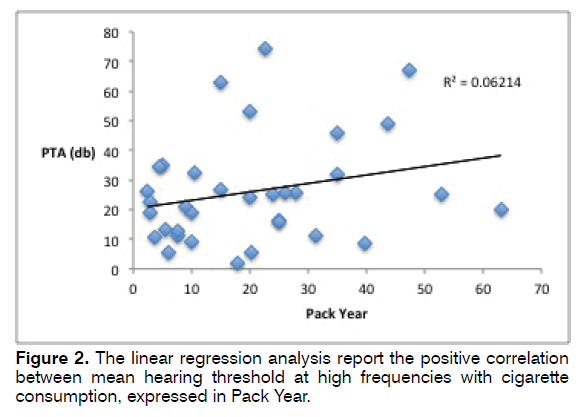
In the smoker group, the amount of cigarettes smoked in lifetime, expressed as mean, was 20.41. Linear regression showed a positive relationship (R² = 0.062) between PTA and Pack-Year, as reported in the regression analysis showed in Figure 2.
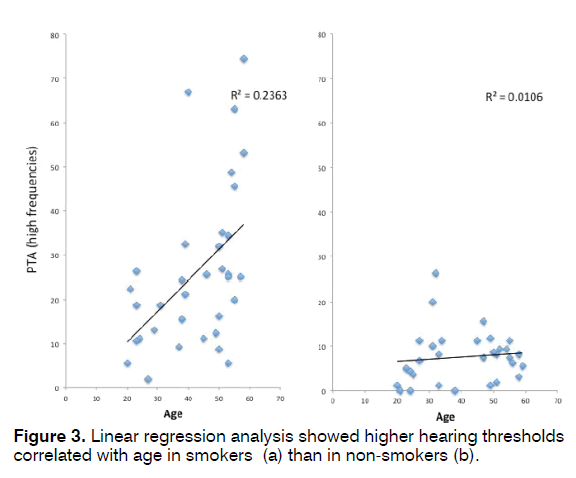
Linear regression analysis showed a significant positive correlation between PTA and age in smokers, with a slope of the regression higher in smokers (R² =0.236) than in non-smokers (R² = 0.0106), showing a higher degree of inner ear suffering with age in smokers, as depicted in Figure 3. Logistic regression including both Pack-Year and age as independent variables was significant (p = 0.015). Linear regression did not show significant association between hypertension and PTA (p = 0.06).
Among smokers, 20 subjects (59%) presented an impaired tubal function in the nine-step inflation/deflation tympanometric test, while only 6(19%) subjects in the group of nonsmokers showed a tubal dysfunction (Table 1); this difference is statistically significant for the chisquare test (p < 0.05). Eustachian tube dysfunction and high frequency hearing loss were not correlated.
Discussion
Smoke and hearing loss
Previous studies reported that smoking is a risk factor for age-related hearing loss and that there is a dose-response relationship with the exposure to tobacco, even after adjusting for age and sex [3].
The subjects included in our study were recruited from a hospital-based tobacco cessation centre, and this may have biased the results. People who seek medical help to quit tobacco may already suffer from cardiovascular disease related to smoking and moreover may be more exposed. However, the average packyears of smoking of our study was 20.41, which can be classified as moderate exposure.
Our result regarding inner ear suffering in smokers confirms the correlation between smoking and hearing loss. As expected, hearing loss is moderate and occurs principally at the higher frequencies, according to the usual aspect of sensorineural hearing loss; therefore, smoke acts at the inner ear as a normal pathogenic factor. The correlation between smoke and hearing loss is strongly supported by the correlation between hearing loss and number of cigarettes per day.
Moreover, we have observed a more important regression of hearing threshold with age in smokers. This pattern suggests that presbycusis could be aggravated by smoking and, therefore, the avoidance of tobacco use could reduce the effects of age on hearing in a worldwide population that is becoming progressively older.
Smoke and Eustachian Tube Function
Another new aspect evaluated in our study is the middle ear function in smokers who are not affected by a clinically manifested otitis media. Until now, data about the possible relationship between otitis media and smoking have been minimal and, above all, based on studies of children exposed to second hand smoke [14,18]. Gaur investigated the presence of middle ear pathologies (chronic suppurative otitis media, acute otitis media, secretory otitis media, and otosclerosis) in a large sample of smokers and found low odds of middle ear diseases (overall odds, 1.13; CI, 0.97 -1.31) [2]. Our starting point was to determine if smokers could have lesser equalisation capability and thus are more prone to developing middle ear diseases or symptoms related to tubal dysfunction such as pressure sensations in the ear, fluctuating hearing loss, or ringing in the ears.
Various tests to measure ET function have been developed, including tympanometry, pneumatic otoscopy, sonotubometry, nine-step test and tubomanometry. However, none has been found to be completely reliable and in clinical practice usually the diagnosis of ETD relies on patient’s history and clinical examination combined with tympanometry [19].
The main problem in exploring eustachian tube is that test available explores its opening under artificial circumstances as a surrogate marker for ET function. In reality, this complex organ has a dynamic functioning and does not necessarily open with each swallowing. Moreover it has also been hypothesized that, similarly to nasal mucosa, fluctuations in mucosal congestion can cause significant changes in tube patency in as little as 1 hour [20]. This is the reason because in general Eustachian Tube Tests shows poor repeatability and may be influenced by short-term fluctuations [21]: even in normal ears, no test is reported to detect opening of the ET in 100% of repeated tests.
In order to carry out an analytical evaluation of the tubal function, we used the nine-step inflation/deflation test, which has the advantage that can be performed with a tympanometer, an instrument that can be found in every institution, and does not need adjunctive and expensive equipment. It is considered a reliable test, as detects ET opening in 81% of normal subjects [21], and easy method for evaluating eustachian tube function; it is normally used to evaluate divers’ middle ear equalisation problems since it is considered a valuable tool to predict middle ear barotrauma [22].
Since this test must be applied with a normal tympanogram, in our study we have excluded from the sample subjects who had evidence of middle ear disorders or an altered basal tympanometry; therefore, we lack data about the prevalence of otitis media in smokers. In our sample, more than half of smokers showed an infraclinical tubal dysfunction without otitis media, a value significantly higher than in the nonsmoker population, suggesting that the toxic effects of smoking could also be present in the tubal mucosa. This suggests that smokers could be more prone to recurrent otitis media and barotrauma due to difficulties in pressure equalisation. The latter point is particularly significant for those who carry out professional or recreational diving. However, more investigations are needed to confirm that this tubal dysfunction could be considered a risk factor for middle ear pathologies.
Limitations
This study is subject to a number of limitations. Our population was small and we don’t have data regarding other associated factors such as alcohol consumption, nutrition, overall health and physical fitness and so on for either subject group. Previous studies suggest that lifestyle factors may moderate the risk of hearing loss, even if alcohol consumption was associated with a protective effect [23]. We assessed the effect of smoking on hearing loss in in selected a population without occupational noise exposure and other risk factors (middle ear pathologies, chronic rhinitis, hypercholesterolemia, diabetes). It is therefore difficult make comparison with the general popuation. However, compared to the results of population-based studies [24] standard non-smokers had better hearing. Also selections of subjects in the study group may have biased the results. In fact the hospital-based tobacco center is a considerably closed community that attracts people with a strong knowledge of the harm of smoking and that can be more subject to atherosclerosis induced damage. Another limitation was that case patients and control subjects were not perfectly matched: age distribution was slightly different between the two groups. A larger epidemiological study based on non-biased cohort of smokers compared with a group of randomly selected participants should be done.
In addition, there are no descriptions of the amount of noise-exposure or other chemical exposure at work or during recreation that could have biased the results. Moreover we used only the nine step inflation and deflation test to evaluate eustachian tube function. Even if this test has shown to be more reliable than the simple tympanometry, shows a poor repeatability and therefore, other test such as tubomanometry or a subjective questionnaire such as the Eustachian Tube Score [25] should have been added to our diagnostic protocol. As shown in previous studies a combination of nine- step test and sonotubometry detected ET opening in 96% of healthy subjects [26].
Conclusion
It seems quite clear from the report above that the harmful effects of cigarette smoking greatly affect the auditory apparatus, as well as promoting the onset of cancer, cardiovascular disease, and respiratory disease. Therefore, tobacco has the power to reduce the ability to hear, mainly causing a sensorineural hearing loss at higher frequencies.
For the first time, the correlation between exposure to cigarette smoking and the good function of the eustachian tube was also thoroughly analysed. In our study, we found the presence of a high number of smokers suffering from tubal dysfunction. This has important clinical relevance, not only because smoking increases the incidence of middle ear diseases, but also because tubal dysfunction may cause in these subjects nonspecific symptoms characterised by ear fullness, subjective loss of hearing, and difficulties in middle ear equalisation. Further studies are needed to confirm our findings and to assess whether there is a positive relation between smoking and symptoms related to tube dysfunction.
Disclosure of interest
The authors declare they don’t have competing interest.
References
- World Health Organization. WHO Report on the Global Tobacco Epidemic. (2013). The MPOWER package. World Health Organization. http://www.who.int/tobacco/mpower/en/.
- Gaur K, Neeraj K, Rajeev G. Association of Smoking or Tobacco Use with Ear Diseases among Men: A Retrospective Study. Tob Induc Dis. 2012;10(1):4.
- Cruickshanks KJ1, Klein R, Klein BE, Wiley TL, Nondahl DM, Tweed TS. Cigarette Smoking and Hearing Loss: the epidemiology of hearing loss study. JAMA. 1998; 279(21):1715-9.
- Mehrparvar AH, Mirmohammadi SJ, Hashemi SH, et al. Concurrent effect of noise exposure and smoking on extended high-frequency pure tone threshold. Int J Audiol. 2015;54(5):301-7.
- Barone JA, Peters JM, Garabrant DH, Bernstein L, Krebsbach R. Smoking as a risk factor in noise-induced hearing loss. J Occup Med. 1997;29(9):741-5.
- Karlsmose B, Lauritzen T, Engberg M, Parving A. A five-year longitudinal study of hearing in a Danish rural population aged 31-50 years. Br J Audiol. 2000;34(1):47-55.
- Talaat HS, Metwaly MA, Khafagy AH, Abdelraouf HR. Dose passive smoking induce sensorineural hearing loss in children? Int J Pediatr Otorhinolaryngol. 2014;78(1):46-9.
- Lan X, Lederman R, Eng JM, Shoshtari SSM, Saleem MA, Malhotra A, et al. Nicotine Induces Podocyte Apoptosis through Increasing Oxidative Stress. PLoS One. 2016;1:11.
- Sumit AF, Das A, Sharmin Z, Ahsan N, Ohgami N, Kato M, et al. Cigarette Smoking Causes Hearing Impairment among Bangladeshi Population. PLoS ONE. 2015;10(3):1-12
- Shimada S, Hasegawa K, Wada H, Terashima S, Satoh-Asahara N, Yamakage H, et al. High blood vis- cosity is closely associated with cigarette smoking and markedly reduced by smoking cessation. Circ J. 2011;75(1):185-9.
- Wild DC, Brewster MJ, Banerjee AR. Noise-induced hearing loss is exacerbated by long-term smoking. Clin Otolaryngol. 2005;30:517-20.
- Starck J, Toppila E, Pyykkö I. Smoking as a risk factor in sensory neural hearing loss among workers exposed to occupational noise. Acta Otolaryngol. 1999;119(3):302-5.
- Blakley BW, Blakley JE. Smoking and middle ear disease: are they related? A review article. Otolaryngol Head Neck Surg. 1995;112(3):441-6.
- Adair-Bischoff CE, Sauve RS, Kimberley B, Brant R. Smoking and middle ear disease. Otolaryngol Head Neck Surg.1996;114(6):837-40.
- Patel MA, Mener DJ, Garcia-Esquinas E, Navas-Acien A, Agrawal Y, Lin SY. Tobacco Smoke Exposure and Eustachian Tube Disorders in US Children and Adolescents. PLoS One. 2016;11(10):e0163926.
- Sharabi Y, Reshef-Haran I, Burstein M, Eldad A. Cigarette smoking and hearing loss: lessons from the young adult periodic examinations in Israel (YAPEIS) database. Isr Med Assoc J. 2002;4(12):1118-20.
- Bluestone CD. Assessment of eustachian tube function. In: Jerger J, ed. Handbook of Clinical Impedance Audiometry. New York, American Electromedics Corporation, 1975.
- Aligne CA, Stoddard JJ. Tobacco and children. Arch Pediatr Adolesc Med. 1997;151(7):648-53.
- Schilder AGM, Bhutta MF, Butler CC, Holy C, Levine LH, Kvaerner KJ, et al. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol. 2015;40(5):407-11.
- Moore M, Eccles R. Normal nasal patency: problems in obtaining standard reference values for the surgeon. J Laryngol Otol. 2012;126(6):563-9.
- Smith ME, Blythe AJ, Baker C, Zou CC, Hutchinson PJA, Tysome JR. Tests of Eustachian Tube Function: the Effect of Testing Technique on Tube Opening in Healthy Ears. Otol Neurotol. 2017;38(5):714-20
- Uzun C, Adali MK, Tas A, Koten M, Karasalihoglu AR, Devren M. Use of the nine-step inflation/deflation test as a predictor of middle ear barotrauma in sports scuba divers. Br J Audiol. 2000;34(3):153-63.
- Dawes P, Cruickshanks KJ, Moore DR, Edmondson-Jones M, McCormack A, Fortnum H, et al. Cigarette smoking, passive smoking, alcohol consumption, and hearing loss. J Assoc Res Otolaryngol. 2014;15(4):663-74.
- Von Gablenz P, Holube I. Hearing threshold distribution and effect of screening in a population-based German sample. Int J Audiol. 2016;55(2):110-25.
- Schröder S, Lehmann M, Sauzet O, Ebmeyer J, Sudhoff H. A Novel Diagnostic Tool for Chronic Obstructive Eustachian Tube Dysfunction-The Eustachian Tube Score. Laryngoscope. 2015;125(3):703-8.
- McBride T, Cunningham M, Derkay C, Doyle W. Evaluation of non-invasive eustachian tube function tests in normal adults. Laryngoscope. 1988;98(6 Pt 1):655-8.
References
1ENT Department, Mauriziano Hospital “Umberto I”, C.so Re Umberto 109, Torino, Italy
2Pneumology Department, Mauriziano Hospital “Umberto I”, C.so Re Umberto 109, Torino, Italy
3Surgical Science Department, University of Torino, Via Genova 3, Torino, Italy
Send correspondence to:
Matteo Pezzoli
Ospedale Mauriziano “Umberto I”, Corso Re Umberto, 109. 10128 Torino, E-mail: ma.pezzoli@libero.it
Paper submitted to the ITJ-EM (Editorial Manager System) on August 08, 2017; and accepted on August 23, 2017.
Citation: Pezzoli M, Lofaro D, Oliva A, Orione M, Cupi D, Albera A, Bongioannini G, Albera R. Effects of Smoking on Eustachian Tube and Hearing. Int Tinnitus J. 2017;21(2):98-103