The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 27, Issue 1 / June 2023
Case Report Pages:58-60
10.5935/0946-5448.20230010
Gradenigo Syndrome in a 6-Year-Old Boy with Acute Otitis Media: A Case Report
Authors: Jaber Ahmed Al-Faifi
PDF
Abstract
Gradenigo Syndrome (GS) is not a common intracranial complication of acute otitis media infections that needs proper diagnosis and management. This case report presents a 6-year-old child diagnosed with unilateral headache, right eye diplopia, and right abducens nerve palsy. MRI and cranial nerve examination facilitate the confirmation of GS. The patient was treated with proper antibiotics and showed good outcomes. This case report highlights the importance of early detection and understanding of the clinical picture associated with GS, which have a crucial role in achieving desired outcomes and avoiding serious complications
Keywords: Otitis media, Diplopia, Middle ear, Otorhinolaryngology
Introduction
Gradenigo Syndrome (GS) is an intracranial acute otitis media infection complication. GS involves an extension of inflammation from the middle ear to the rock tip and tissues near the cranial nerves with increasing severity. It is caused by aerobic gram-negative rod bacteria (Klebsiella pneumoniae, Escherichia coli, Pseudomonas aeruginosa, Hemophilus influenzae, and Moraxella catarrhalis). The anaerobic bacterium Fusobacterium necrophorum may also be found [1-4].
GS tends to occur in the pediatric population at an average age of 12, with a mortality rate between 2% and 2.6% [3]. Otorrhea, facial or retroorbital pain that spreads to the trigeminal nerve and paralysis of the abducens nerve are characteristic of this condition. GS is a serious condition because it is close to the middle ear and the initial symptoms are not specific [5].
With the widespread use of antibiotic agents, GS complications have become extremely rare. However, inappropriate clinical assessment and management can lead to life-threatening consequences [5, 6]. This study reports a 6-year-old boy with unilateral headache, diplopia of the right eye, and paralysis of the right abducens nerve, diagnosed as GS.
Case Report
Previously healthy 6-year-old Saudi boy from a remote village outside Bisha Province was brought by his nonconsanguineous parents and admitted to the Maternity and Children’s Hospital (MCH) in Bisha, Saudi Arabia. He had complaints of unilateral headache, vomiting, and right-eye diplopia. The patient’s medical history indicated an upper respiratory tract infection (pharyngitis) that had been diagnosed at a local health center (PHC) in the previous three weeks. The disease was associated with high fever and was treated with 500 mg of amoxicillin orally every 8 hours (80 mg/kg/day for 5 days), and 281 mg of acetaminophen orally every 6 hours (15 mg/kg/day for 5 days). The boy’s condition gradually improved, but one week later, he started vomiting and having headaches. He was diagnosed at the PHC with acute otitis media and started on topical antibiotics. Ear drops were used for five days and then stopped.
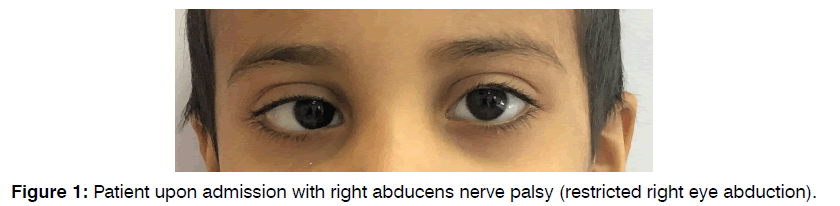
Due to persistent complaints, he brought to MCH with complaints of unilateral headache, vomiting, and new-onset right-eye diplopia (Figure 1). Upon clinical examination, he was vitally stable and afebrile, with signs of mild dehydration due to frequent vomiting. A neurological analysis indicated no signs of meningeal irritation with average power, tone, and deep tendon reflexes. The cranial nerve examination was routine apart from right-abducens nerve palsy. Other physical and neurological tests were unremarkable.
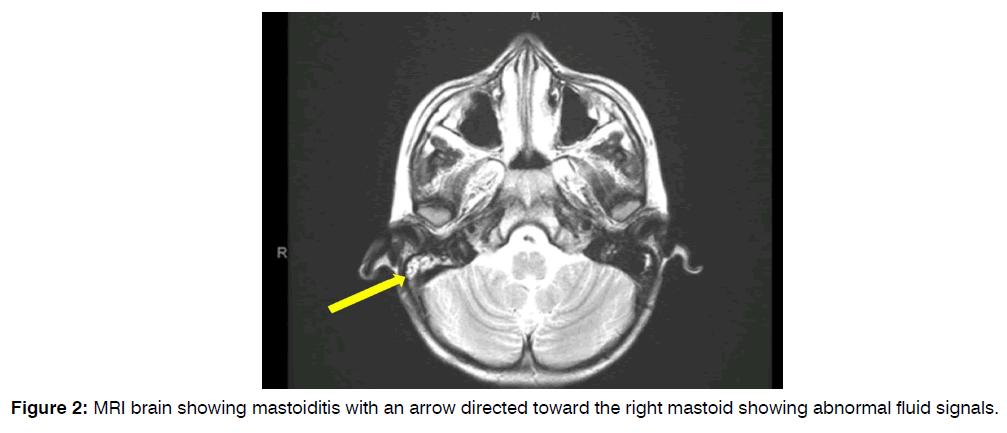
Otorhinolaryngologic findings confirm the presence of right-side acute otitis media. The tympanic membrane is hyperemic and bulging. Funduscopic examination was normal. Laboratory results showed a white blood cell count of 6140/mm3, a platelet count of 256,000/mm3, and a C-reactive protein level of less than six mg/l. An MRI scan of the brain with contrast was requested and showed abnormal fluid signals in the air cells of the right mastoid with suspected mastoiditis (Figure 2).
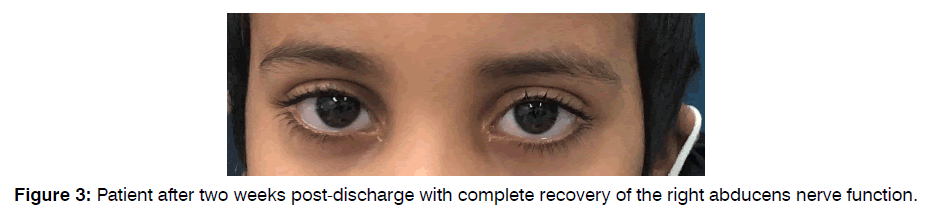
The patient was hospitalized and received ceftriaxone and metronidazole, which he took for ten days. Intravenous hydrocortisone was also started at 47 mg every 12 hours (5 mg /kg/day) and continued for five days. After admission, the vomiting and headache began to improve until discharge after ten days with the patient in better condition (Figure 3). After two weeks, the patient was followed up at the outpatient clinic and showed complete recovery of proper abducens nerve function.
Discussion
In 1904, Giuseppe Gradenigo stated that GS is the classic trial of otorrhea, retro-orbital pain, and paralysis of the sixth nerve [7, 8]. However, the classic triad may be different [7]. The way that GS works is that bacteria in the middle ear spread to the air cells of the mastoid bone and then to the petrous temporal bone [5] Because of its proximity to neurovascular structures, the infection may spread to Dorello’s canal and affect the abducens nerve, inferior petrosal sinus, and Meckel’s sinus. The anatomic area contains the ganglion of the trigeminal nerve [8].
The clinical manifestations of GS arise from inflammatory phlegm when compression or irritation of the abducens and trigeminal nerves produces the triad of symptoms recognized by Gradenigo [3, 6]. Infiltration may originate from the air cells of the mastoid or sphenoid bone or the lymphatic vessels, involving the mucosa of the apical rock cells of the temporal bone [3]. The presentation of this case is mainly headache, vomiting, new-onset diplopia of the right eye, and paralysis of the right abducens nerve. In addition, acute otitis media with a hyperemic and bulging tympanic membrane were present. Evidence indicates that the presence of fever, headache, and photophobia associated with unilateral abducens nerve palsy is of clinical concern [9]. However, in the scientific literature, classic GS is defined as the presence of otitis media, abducens nerve palsy, and facial pain in the trigeminal region [3].
In addition to clinical presentations, radiological confirmation of petrous apicitis plays a crucial role in diagnosing GS [3]. It is well known that MRI has a significant role in detecting otitis media complications and assessing inflammatory soft tissue changes [4, 6]. MRI revealed abnormal fluid signals in the right mastoid in the present case. Therefore, contrast-enhanced MRI and magnetic resonance venography must be performed immediately in patients with neurologic symptoms such as nerve palsy, neck stiffness, or confusion [4].
In most GS cases, medical management is helpful, and surgical intervention is typically reserved for cases of delayed response. In the absence of life-threatening complications and chronic year infections, antibiotic treatment of GS is the best choice and can achieve desired outcomes [3, 6]. Evidence shows that administering broad-spectrum antibacterial agents might be effective against several types of microorganisms that cause mastoiditis. However, if the diagnosis is delayed or if the antibiotics are not responsive, then mastoidectomy and temporal bone epicectomy may be necessary [9].
Empirical antibiotic treatment should act against various causative agents, including aerobic and non-anaerobic microorganisms [2, 6]. In the present case, the patient responded well to ceftriaxone and metronidazole. Cephalosporin and metronidazole, with or without adding vancomycin, have already been shown to be effective drugs for treating GS2. Furthermore, steroids reduce inflammation, edema, and nerve compression [7].
Conclusion
The present case report highlights the importance of GS as a rare condition that needs special attention throughout the clinical examination, diagnosis, and management. Early detection and understanding of the clinical features associated with GS are crucial in reaching the desired outcome and voiding serious complications.
References
- McLaren J, Cohen MS, El Saleeby CM. How well do we know Gradenigo? A comprehensive literature review and proposal for novel diagnostic categories of Gradenigo's syndrome. Int J Pediatr Otorhinolaryngol. 2020;132:109942.
- Sousa Menezes A, Ribeiro D, Balona F, Maré R, Azevedo C, Rocha J, et al. Gradenigo’s syndrome with carotid septic stenosis. Case Rep Otolaryngol. 2020.
- Bonavia L, Jackson J. Gradenigo Syndrome in a 14-Year-old Girl as a Consequence of Otitis Media with Effusion. J Neuroophthalmol. 2022;42(1):e408.
- Özkaçmaz S. Acute otitis media associated with Gradenigo syndrome and transverse sinus thrombosis: a case report. J Int Med Res. 2019;47(3):1348-52.
- Costa JV, João M, Guimarães S. Bilateral papilledema and abducens nerve palsy following cerebral venous sinus thrombosis due to Gradenigo's syndrome in a pediatric patient. Am J Ophthalmol Case Rep. 2020;19:100824.
- Quesada J, Kong A, Tweddle E. An unusual case of acute otitis media resulting in Gradenigo syndrome: CT and MRI findings. Radiol Case Rep. 2021;16(12):3903-7.
- Liu Y, Yeh PK, Lin YP, Sung YF. Steroid-Responsive gradenigo’s syndrome mimicking subdural hematoma. Cureus. 2021;13(11).
- Bano S, Nawaz A, Asmar A, Rehman MA, Farooq H, Ali H. Gradenigo's syndrome presenting as IX and X cranial nerve palsy without clinically apparent ear infection: A case report and review of literature. Eneurologicalsci. 2022;27:100397.
- Athapathu AS, Bandara ER, Aruppala AA, Chandrapala KM, Mettananda S. A child with Gradenigo syndrome presenting with meningism: A case report. BMC Pediatr. 2019;19(1):1-3.
Assistant Professor of Pediatrics, Department of Child Health, College of Medicine, University of Bisha, Bisha, Saudi Arabia
Send correspondence to:
Jaber Ahmed Al-Faifi
Assistant Professor of Pediatrics, Department of Child Health, College of Medicine, University of Bisha, Bisha, Saudi Arabia, Email jalfaifi@ub.edu.sa
Tel 556765771.
Paper submitted on April 11, 2023; and Accepted on April 17, 2023
Citation: Al-Faifi JA. Gradenigo Syndrome in a 6-Year-Old Boy with Acute Otitis Media: A Case Report. Int Tinnitus J. 2023;27(1):58-61.