The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 24, Issue 2 / December 2020
Research Article Pages:102-107
10.5935/0946-5448.20200020
Proprioception: the missing link in the pathogenesis of tinnitus?
Authors: Henk M Koning
PDF
Abstract
Objectives: The object of this study was to relate cervical spine pathology to the occurrence of tinnitus and of cervical pain.
Design: A retrospective analysis of 124 patients with tinnitus as main complaint and 300 patients with cervical pain as main complaint who visited our clinic in a two-year period.
Results: In patients with tinnitus as main complaint, 64% of the patients have also cervical pain, and in patients with cervical pain as main complaint, 44% of the patients have tinnitus. Both groups of patients have in common a high prevalence of postural instability and dizziness, degeneration of the intervertebral disc between the fifth and seventh cervical vertebrae, and a large anterior spur in front of the fifth cervical vertebrae. Patients with cervical pain as main complaint have more degeneration of the intervertebral disc between the third and fourth cervical vertebrae, a larger anterior spur in front of the third cervical vertebrae and more loss of cervical lordosis.
Conclusions: Postural instability is an important discriminant factor in patients with cervical pain and in patients with tinnitus as main complaint. In patients with cervical pain postural instability was associated with the occurrence of tinnitus. In patients with tinnitus, there is evidence for two profiles of somatic tinnitus, discriminated by the occurrence of postural instability and low-frequency hearing loss. It seems that the combination of tinnitus and postural instability begins as a cervical pain syndrome and that the tinnitus aggravates in time, possibly by the occurrence of hearing loss, internal diseases, or surgery of the lower limb
Keywords: Tinnitus, cervical spondylosis, proprioception, cuneate nucleus, postural instability
Introduction
Cervical spine disorders can initiate not only cervical pain but also tinnitus [1,2]. Cervical spondylosis is an age-related chronic degenerative condition of the cervical spine, which can cause neck pain and functional limitations [1]. The usual occurrence is at C5-C6 and C6-C7 levels, although higher levels may also be involved. In patients with tinnitus, the second (C2), the fifth (C5), and the eight (C8) cervical nerve are the most prominent involved in the pathogenesis of tinnitus [2]. Separate cervical spinal pathology might cause cervical pain or tinnitus. The object of this study was to relate cervical spine pathology to the occurrence of tinnitus and of cervical pain. We did so by comparing patients with cervical pain with patients with tinnitus as main symptom.
Methods
The Medical research Ethics Committees United (Nieuwegein, the Netherlands) approved the present observational retrospective study.
Subjects: All patients who visited our clinic for cervical pain or for tinnitus in a two years interval (from 1/1/2018 to 31/12/2019) participated in the study. The work-up of patients consisted of a standardized clinical history, and a cervical spine radiograph. The standardized clinical history included duration of complaints and age of onset, the visual analogue scale (VAS) of the main complaint, and concomitant symptoms (the presence of postural instability, dizziness, tinnitus and cervicalgia). The lateral cervical spine radiographs were assessed for the angle between the posterior border of the third and sixth cervical vertebrae, the intervertebral disc space height from the second till the seventh cervical vertebrae, and the size of the anterior osteophyte of the third till the sixth cervical vertebrae, as previously described [3].
Statistical Methods: Statistical analysis was performed with Minitab 18 (Minitab Inc., State College, PA, USA). Student’s t-test was used for continuous variables and χ2 test was used for dichotomous variables. A p-value less than 0.05 was considered statistically significant.
Results
In a two-year period, 124 patients visit our clinic with tinnitus as main complaint and 300 patients with cervical pain as main complaint. The aspects of the patient’s groups are compared in Table 1. In patients with tinnitus as main complaint, 64% of the patients have also cervical pain, and in patients with cervical pain as main complaint, 44% of the patients have tinnitus. Both groups of patients have in common a high prevalence of postural instability and dizziness, degeneration of the intervertebral disc between the fifth and seventh cervical vertebrae, and a large anterior spur in front of the fifth cervical vertebrae. Patients with cervical pain as main complaint have more degeneration of the intervertebral disc between the third and fourth cervical vertebrae, a larger anterior spur in front of the third cervical vertebrae and more loss of cervical lordosis. Patients with tinnitus as main complaint are more male and older at the start of tinnitus.
| Tinnitus as main complaint (n=124) | Cervical pain as main complaint (n=300) | P-value | |||||
| Prev. | Mean | SEM | Prev. | Mean | SEM | ||
| Gender (male) | 57% | 32% | 0.000 Sign. | ||||
| Postural instability | 42% | 54% | 0.027 Sign. | ||||
| Dizziness | 45% | 52% | 0.199 | ||||
| Cervical pain | 64% | 100% | 0.000 Sign. | ||||
| Tinnitus | 100% | 44% | 0.000 Sign. | ||||
| Age at the start of the complaint (year) | 47 | 1.3 | 41 | 1.4 | 0.001 Sign. | ||
| Angle between vertebrae C2 and C6 (degrees): | 7 | 0.9 | 4 | 0.6 | 0.014 Sign. | ||
| Farfan’s measurement of disc space height (%): | |||||||
| - C2-C3 | 38 | 0.6 | 37 | 0.5 | 0.057 | ||
| - C3-C4 | 35 | 0.7 | 33 | 0.5 | 0.008 Sign. | ||
| - C4-C5 | 33 | 0.7 | 32 | 0.5 | 0.114 | ||
| - C5-C6 | 26 | 0.8 | 27 | 0.6 | 0.703 | ||
| - C6-C7 | 26 | 0.9 | 25 | 0.5 | 0.576 | ||
| Size of anterior osteophyte (%): | |||||||
| - C3 | 8 | 0.4 | 10 | 0.4 | 0.000 Sign. | ||
| - C4 | 12 | 0.7 | 13 | 0.4 | 0.237 | ||
| - C5 | 19 | 0.7 | 18 | 0.5 | 0.534 | ||
| - C6 | 15 | 0.6 | 14 | 0.5 | 0.930 | ||
Table 1: Patients with tinnitus as main complaint were compared with patients with cervical pain as main complaint.
Patients with cervical pain as main complaint: In patients with cervical pain as main complaint, the presence of tinnitus was related with postural instability and dizziness. In patients with cervical pain as main complaint and postural instability, 58% of the patients report tinnitus compared to 26% in the other patients. Statistical analysis indicates that a higher VAS of the minimal cervical pain (p=0.005), a higher VAS of the mean cervical pain (p=0.11), and a larger anterior spur at the sixth cervical vertebrae (p=0.006) were statistically significant related to the prevalence of postural instability in patients with cervical pain. A VAS of the minimal pain more than 30 millimetre raises the manifestation of postural instability from 45% to 63%. An anterior spur at the sixth cervical vertebrae larger than 14 % increases the incidence of postural instability from 48% to 63% (Table 2).
| Tinnitus (n=129) | No tinnitus (n=167) | P-value | |||||
| Prev. | Mean | SEM | Prev. | Mean | SEM | ||
| Gender (male) | 33% | 31% | 0.609 | ||||
| Postural instability | 72% | 40% | 0.000 Sign. | ||||
| Dizziness | 65% | 42% | 0.000 Sign. | ||||
| VAS pain | |||||||
| - Mean | 59 | 3.2 | 56 | 2.3 | 0.429 | ||
| - Minimal | 35 | 3.3 | 29 | 2.1 | 0.085 | ||
| - Maximal | 85 | 1.3 | 85 | 1.3 | 0.898 | ||
| Angle between vertebrae C2 and C6 (degrees): | 4 | 0.9 | 4 | 0.8 | 0.967 | ||
| Farfan’s measurement of disc space height (%): | |||||||
| - C2-C3 | 37 | 0.7 | 36 | 0.6 | 0.314 | ||
| - C3-C4 | 32 | 0.7 | 33 | 0.7 | 0.866 | ||
| - C4-C5 | 32 | 0.7 | 32 | 0.7 | 0.917 | ||
| - C5-C6 | 26 | 0.9 | 27 | 0.8 | 0.221 | ||
| - C6-C7 | 25 | 0.8 | 26 | 0.7 | 0.302 | ||
| Size of anterior osteophyte (%): | |||||||
| - C3 | 11 | 0.6 | 9 | 0.4 | 0.056 | ||
| - C4 | 13 | 0.7 | 12 | 0.5 | 0.173 | ||
| - C5 | 18 | 0.7 | 18 | 0.7 | 0.876 | ||
| - C6 | 15 | 0.7 | 14 | 0.6 | 0.573 | ||
Table 2: Patients with tinnitus were compared with patients with no tinnitus in the group of patient with cervical pain as main complaint.
Patients with tinnitus as main complaint: Postural instability is found in 42% of the patients with tinnitus as main complaint. These patients had a prevalence of more female, more cervical pain, more heart and vascular diseases, more other internal medical disorders, more use of analgesics, and more hearing loss from 250 Hz till 1 kHz. Tinnitus patients without postural instability were more men with hearing loss from 2 kHz till 8 kHz, less cervical pain, healthier, and more surgery of shoulders, arms and hands.
Discussion
Our study indicates that postural instability is a discriminant factor in patients with cervical pain and in patients with tinnitus as main complaint. In patients with cervical pain postural instability was associated with the occurrence of tinnitus. In patients with tinnitus, there is evidence for two profiles of somatic tinnitus, discriminated by the occurrence of postural instability and low-frequency hearing loss. It seems that the combination of tinnitus and postural instability begins as a cervical pain syndrome and that the tinnitus aggravates in time, possibly by the occurrence of hearing loss, internal diseases, or surgery of the lower limb.
Postural stability is dependent on complex interactions between the proprioceptive, visual and vestibular sensory systems [4]. Dysfunction in any of these systems cause decreased stability or dizziness. Besides central vestibular disorders and peripheral neuropathy, proprioception might be disrupted as a result of traumatic damage of tissues, muscle fatigue and/or the activation of nociceptors [1,5]. Cervical proprioception is impaired in subjects with cervical spondylosis and it is known to correlate with neck pain intensity [1]. In our study, a VAS of the minimal cervical pain over 30 millimetre and an anterior spur at the sixth cervical vertebrae larger than 14% raise the occurrence of postural instability significantly.
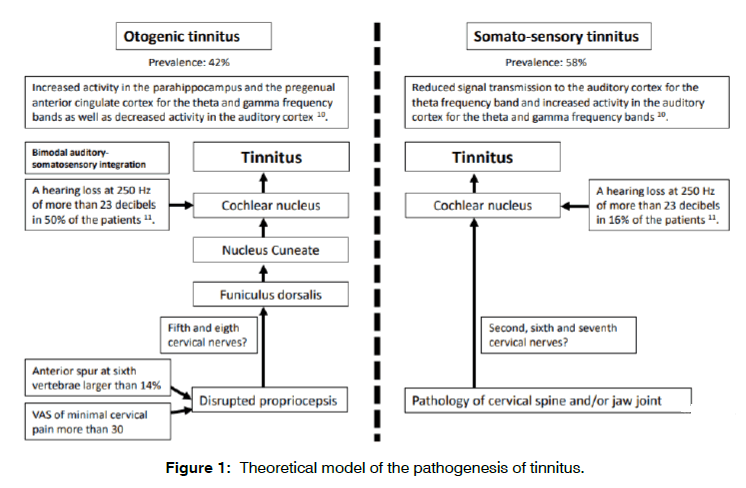
Unconscious proprioception is detected through primary sensory afferents innervating receptors in joints, muscle, and skin [6]. The proprioceptive and mechanoreceptive projections from the larger, myelinated DRG neurons ascend in the ipsilateral dorsal funiculus to the gracile and cuneate nucleus of the brainstem. Both nuclei transmit their information to the cochlear nucleus. In the cochlear nucleus bimodal auditory-somatosensory integration takes place and reduction of the auditory input leads to more excitatory somatosensory input to the cochlear nucleus [7]. In our study, disrupted proprioception was the important somatosensory input leading to tinnitus in patients with cervical pain.
Our findings in patients with tinnitus as main complaint provide evidence for two profiles of somatic tinnitus, discriminated by the occurrence of postural instability. In patients with tinnitus, postural instability was associated by a high prevalence of female gender, cervical pain, heart and vascular diseases, and significant hearing loss from 250 Hz till 1 kHz. In patients with this subtype of tinnitus, it seems that cross-modal interactions between auditory and somatosensory systems appear to take place within in the auditory pathway [8]. Hearing loss together with an impaired proprioception are the triggers for the perception of tinnitus in this subtype of tinnitus. The combination of tinnitus and postural instability might begin as a cervical pain syndrome and it is possible that the tinnitus aggravates in time, possibly by the occurrence of hearing loss, internal diseases, or surgery of the lower limb.
The group of somatic tinnitus without postural instability consists of patients often male, with cervical pain, with hearing loss from 2 kHz till 8 kHz, and cervical disc degeneration from C5 to C7 with an anterior spur at the fifth cervical vertebrae. Activation of the cervical nervous system, especially the dorsal root ganglia, can cause disinhibition of the cochlear nucleus eventually resulting in tinnitus [9]. In this subgroup of tinnitus patients, perception of tinnitus might be a direct effect of cervical pathology on the cochlear nucleus. However, we found no radiologic differences of the cervical spine between tinnitus patients with or without postural instability [9] (Table 3).
| Postural instability (n=52) | Intact balance (n=72) | P-value | |||||
| Prev. | Mean | SEM | Prev. | Mean | SEM | ||
| Gender (male): | 40% | 69% | 0.001 Sign. | ||||
| Cervical pain: | 75% | 56% | 0.025 Sign. | ||||
| Heart and vascular disease: | 31% | 10% | 0.002 Sign. | ||||
| Other internal diseases: | 43% | 22% | 0.013 Sign. | ||||
| Surgery of Ankle or Feet: | 20% | 8% | 0.067 Sign. | ||||
| VAS Tinnitus | |||||||
| Mean | 65 | 4.0 | 64 | 2.9 | 0.946 | ||
| Minimal | 38 | 4.7 | 43 | 3.6 | 0.367 | ||
| Maximal | 84 | 2.7 | 80 | 2.5 | 0.310 | ||
| Angle between vertebrae C2 and C6 (degrees): | 5 | 1.3 | 7 | 1.2 | 0.252 | ||
| Farfan’s measurement of disc space height (%): | |||||||
| - C2-C3 | 38 | 1.0 | 38 | 0.8 | 0.930 | ||
| - C3-C4 | 34 | 1.1 | 35 | 1.0 | 0.491 | ||
| - C4-C5 | 32 | 1.0 | 34 | 1.0 | 0.291 | ||
| - C5-C6 | 27 | 1.2 | 26 | 1.1 | 0.629 | ||
| - C6-C7 | 26 | 1.2 | 26 | 1.2 | 0.940 | ||
| Size of anterior osteophyte (%): | |||||||
| - C3 | 8 | 0.5 | 8 | 0.5 | 0.780 | ||
| - C4 | 13 | 1.0 | 11 | 0.9 | 0.205 | ||
| - C5 | 19 | 1.0 | 18 | 1.0 | 0.342 | ||
| - C6 | 15 | 0.9 | 14 | 0.7 | 0.613 | ||
| Hearing loss (dB) at: | |||||||
| - 250 Hz | 27 | 3.0 | 16 | 1.7 | 0.002 Sign. | ||
| - 500 Hz | 27 | 3.1 | 16 | 1.8 | 0.002 Sign. | ||
| - 1 kHz | 29 | 3.1 | 17 | 1.7 | 0.001 Sign. | ||
| - 2 kHz | 33 | 3.0 | 26 | 4.7 | 0.198 | ||
| - 4 kHz | 45 | 3.5 | 41 | 2.7 | 0.351 | ||
| - 8 kHz | 52 | 4.0 | 50 | 3.0 | 0.742 | ||
Table 3: Patients with postural instability were compared with patients with intact balance in the group of patient with tinnitus as main complaint.
In literature, there are indications that there are two types of tinnitus, depending on the amount of hearing loss [10,11]. For tinnitus patients with hearing loss, increased activity in the parahippocampus and the pregenual anterior cingulate cortex for the theta and gamma frequency bands were found as well as decreased activity in the auditory cortex 10. In tinnitus patients with normal hearing there is a reduced signal transmission to the auditory cortex for the theta frequency band and an increased activity in the auditory cortex for the theta and gamma frequency bands. This finding could indicate a deficient noise cancelling mechanism oscillating at non-activated resting state theta frequencies. Another study found also indications for two subtypes of tinnitus, depending on the amount of hearing loss [11]. A form associated with hearing loss, named otogenic tinnitus, and a form caused by somatic disorders involving the head and upper neck. Patients with a hearing loss of more than 23 decibels at 250 Hz were characterized by a high prevalence of selfperceived hearing loss (92% of the patients), balance disorders (75% of the patients), and vertigo (63% of the patients). There is close resemblance with the subtypes we found in this study. Also, the cervical innervation of the auditory pathway showed two distinctive patterns of auditory response for each cervical nerve in patients with tinnitus [2]. Auditory-somatosensory integration is found in C5 and possible C8. However, for cervical nerves C2, C6 and C7 there is no evidence of auditory-somatosensory integration and the involvement of each of these nerve is not associated with hearing loss.
Based on this information, we can hypotheses that there are two types of tinnitus, differentiated by hearing loss, postural instability, or cerebral activity (Figure 1). These subtypes have a different cervical nerve transmission, with one type implying bimodal auditory-somatosensory integration, and the other type with a direct effect of cervical pathology on the cochlear nucleus. It is possible that both subtypes of tinnitus are not mutually exclusive and with a kind of overlap.
This study has some limitations. A first limitation was that there was no audiogram present in patients with cervical pain as main complaint. With these data, conclusions might be taken about relations between disrupted proprioception and the occurrence of hearing loss. A second limitation was that there was no VAS of cervical pain in patients with tinnitus as main complaint. The VAS of cervical pain was related to postural instability in cervical pain patients, and this finding could not be assessed in patients with tinnitus. Future prospective studies are needed with audio graphic testing in cervical pain patients and with an assessment of the VAS of cervical pain in patients with tinnitus.
Conclusion
Postural instability is an important discriminant factor in patients with cervical pain and in patients with tinnitus as main complaint. In patients with cervical pain postural instability was associated with the occurrence of tinnitus. In patients with tinnitus, there is evidence for two profiles of somatic tinnitus, discriminated by the occurrence of postural instability and low-frequency hearing loss. It seems that the combination of tinnitus and postural instability begins as a cervical pain syndrome and that the tinnitus aggravates in time, possibly by the occurrence of hearing loss, internal diseases, or surgery of the lower limb.
Conflict of Interest
There are no conflicts of interest in terms of the present study.
References
- Reddy RS, Tedla JS, Dixit S, Abohashrh M. Cervical proprioception and its relationship with neck pain intensity in subjects with cervical spondylosis. BMC Musculoskelet Disord. 2019;20:447-54.
- Koning HM. Cervical Nerve Projections to the Auditory Pathway in Tinnitus. Int. Tinnitus J. 2020;24(2):68-72.
- Koning HM, Koning MV, Koning NJ, Ter Meulen BC. Anterior Cervical Osteophytes and Sympathetic Hyperactivity in Patients with Tinnitus: Size Matters. Int. Tinnitus J. 2018;22:97-102.
- Cullen K. Vestibular processing during natural self-motion: implications for perception and action. Nat Rev Neurosci. 2019; 20(6): 346-63.
- Malmström E, Fransson P, Bruinen TJ, Facic S, Tjernström F. Disturbed cervical proprioception affects perception of spatial orientation while in motion. Exp Brain Res. 2017;235(9):2755-66.
- Attwell CL, van Zwieten M, Verhaagen J, Mason MRJ. The Dorsal Column Lesion Model of Spinal Cord Injury and Its Use in Deciphering the Neuron?Intrinsic Injury Response. Dev Neurobiol. 2018;78(10):926-51.
- Dehmel S, Pradhan S, Koehler S, Beldsoe S, Shore S. Noise overexposure alters long-term somatosensory-auditory processing in the dorsal cochlear nucleus--possible basis for tinnitus-related hyperactivity? J Neurosci. 2012;32(5):1660-71.
- Dehmel S, Cui YL, Shore SE. Cross-modal interactions of auditory and somatic inputs in the brainstem and midbrain and their imbalance in tinnitus and deafness. Am J Audiol. 2008;17:193-209.
- Bressi F, Casale M, Papalia R, Moffa A, Di Martino A, Miccinilli S, et al. Cervical spine disorders and its association with tinnitus: The "triple" hypothesis. Med Hypotheses. 2017;98:2-4.
- Vanneste S, Alsalman O, De Ridder D. Top-down and Bottom-up Regulated Auditory Phantom Perception. J Neurosci. 2019;39(2):364-78.
- Koning MEJ, Koning HM. Hearing Loss at 250 Hz Can Differentiate Between Different Subtypes of Tinnitus: A Retrospective Chart Review. Int. Tinnitus J. 2018;22(2):170-4.
Department of Pain Therapy, Pain Clinic De Bilt, Netherlands
Send correspondence to:
Henk M Koning
Department of Pain Therapy, Pain Clinic De Bilt, The Netherlands, E-mail: hmkoning@pijnkliniekdebilt.nl Phone: +0031302040753
Paper submitted on November 25, 2020; and Accepted on December 10, 2020
Citation: Proprioception: the missing link in the pathogenesis of tinnitus? 24(2):102-107