The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 27, Issue 2 / December 2023
Research Article Pages:242-246
10.5935/0946-5448.20230037
Recurrent Cholesteatoma: Why It Occurs?
Authors: Fathmath Shana Mohamed, Farah Liana Lokman, Wan Nabila Binti Wan Mansoor, Nadhirah Binti Mohd Shakri, Rizuana Iqbal Hussain, Asma Abdullah
PDF
Abstract
A cholesteatoma is an expansion of keratinizing squamous epithelium that enters the middle ear cleft from the outer layer of the tympanic membrane or ear canal. Choleatomas are always treated surgically. Recurrence of the illness presents another challenge for the patient and the surgeon, though. There have been reports of recurrence rates as high as 30% in adults and as high as 70% in children. Here, we describe a case of persistent recurrent otorrhea following revision surgery, along with acquired recurrent cholesteatoma following canal wall down surgery. Case presentation: A 38-year -male with underlying Diabetes Mellitus and Hypertension presented with left scanty and foul-smelling ear discharge for 2 years and left reduced hearing. He was diagnosed with left chronic active otitis media with cholesteatoma for which he underwent left modified radical mastoidectomy, meatoplasty and tympanoplasty in 2017. Five months post operatively, he presented with left otorrhea. However, he defaulted followed up and presented in April 2018 for similar complaints. Otoscopy examination revealed left tympanic membrane perforation at poster superior quadrant of pars tensa and bluish discoloration behind pars flacida. He was diagnosed as recurrent left cholesteatoma and subsequently he underwent left mastoid exploration under general anesthesia in June 2018. Post-surgery, he developed recurrent ear discharge which was treated with topical antibiotics and ear toileting. Conclusions: We report a case of recurrent Cholesteatoma despite canal wall down procedure requiring a second redo procedure and with persistent recurrent otorrhea after the redo procedure. However, this case demonstrates the need for regular follow ups even after a canal wall down procedure for detecting recurrence of disease. Moreover, this case denotes some of the patient factors and surgeon factors involved in disease recurrence. Furthermore, importance of opting for an imaging study in case of high suspicion of the disease.
Keywords: Recurrent Cholesteatoma, Canal Wall down Procedure, Disease Recurrence, Chronic Ear Discharge, Case Report.
Introduction
Cholesteatoma is a growth of keratinizing squamous epithelium originating from the external layer of the tympanic membrane or ear canal that invades the middle ear cleft [1].
It is well known for its aggressive bone-eroding properties and for its secondary infection that can cause ear discharge. Congenital or acquired cholesteatomas are the two types, with the latter occurring more commonly. Cholesteatoma affects roughly 3 out of every 100,000 children and 12 out of every 100,000 adults. Congenital cholesteatomas, which account for only 2% to 5% of all cholesteatomas, are less common than acquired cholesteatomas.
If cholesteatoma is not treated, it can spread to the mastoid and erode its bony septations. It can also erode the middle ear’s ossicles, leading to conductive hearing loss. Moreover, it may weaken the bone barriers separating the cranial structures from the inner ear, which could result in intracranial and inner ear problems.
The treatment of cholesteatoma is always surgery. However, recurrence of disease is another dilemma for both the surgeon and the patient. Recurrence rates of up to 30% in adults and up to 70% in children have been reported. It is also very important to understand that cholesteatoma recidivism which includes both recurrent and residual Cholesteatoma [2]. While residual cholesteatoma results from incomplete surgical removal of the cholesteatoma matrix, recurrent cholesteatoma results from the reformation of the retraction pocket after a complete previous surgical cholesteatoma removal and recidivism refers to the combination of recurrent and residual disease.
Hence, we report a case of acquired recurrent cholesteatoma after a canal wall down surgery with persistent recurrent otorrhea after the revision surgery.
Case Report
A 38-year male with underlying diabetes mellitus and hypertension presented with left scanty and foul-smelling ear discharge for 2 years and gradual onset of left reduced hearing loss. There was no history of tinnitus, vertigo, and facial asymmetry, recent history of upper respiratory tract infection or features of allergic rhinitis. Otoscopy examination of left ear shows marginal perforation at poster superior quadrant of tympanic membrane extending to posterior canal wall with granulation tissue and active pus discharge. Pars tensa was retracted. Pure Tone Audiometry (PTA) showed right ear normal hearing and left moderate mixed hearing loss Figure 1.
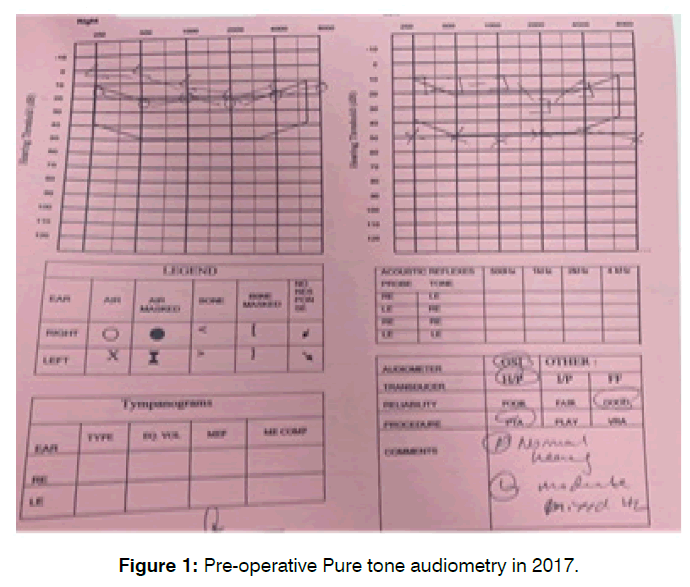
Figure 1: Pre-operative Pure tone audiometry in 2017.
He underwent left modified radical mastoidectomy, meatoplasty and tympanoplasty in March 2017. Intra operative findings showed marginal perforation at the posterior pars tensa, cholesteatoma seen at the antrum, attic and middle ear, granulation tis-sue seen at the mastoid air cells and middle ear. The ossicles; incus was eroded, malleus and stapes were intact. Post operatively, he did not develop any complications and was discharged with advised to follow up after 1 week.
One month post operatively, he complained of left otorrhea which was reddish to yellowish in color, fever, and headache. No other symptoms to suggest intratemporal or intracranial complication. He was treated with corticosteroid nasal spray and antibiotic ear drops and advised to follow up after 1 week. He developed left otorrhea again five months after surgery. During otoscopy, the pars tensa was intact and the mastoid antrum was well epithelized. On the other hand, there were two perforations over the pars flacida and attic whereby the cholesteatomas were all over the attic. But he neglected to follow up.
One year later, in April 2018, he went back to the ENT clinic due to intermittent, yellowish ear discharge from his left ear that persisted for four months and was accompanied by diminished left side hearing. No prior history of upper respiratory tract infection symptoms, fever, tinnitus, headache, facial weakness, or otalgia was present. Otoscopy examination revealed left tympanic membrane perforation at poster superior quadrant of pars tensa and bluish discoloration behind pars flacida. The mastoid bowl was well epithelized. Pure tone audiometry Audiometry revealed right ear normal hearing and left ear moderate mixed hearing loss Figure 2.
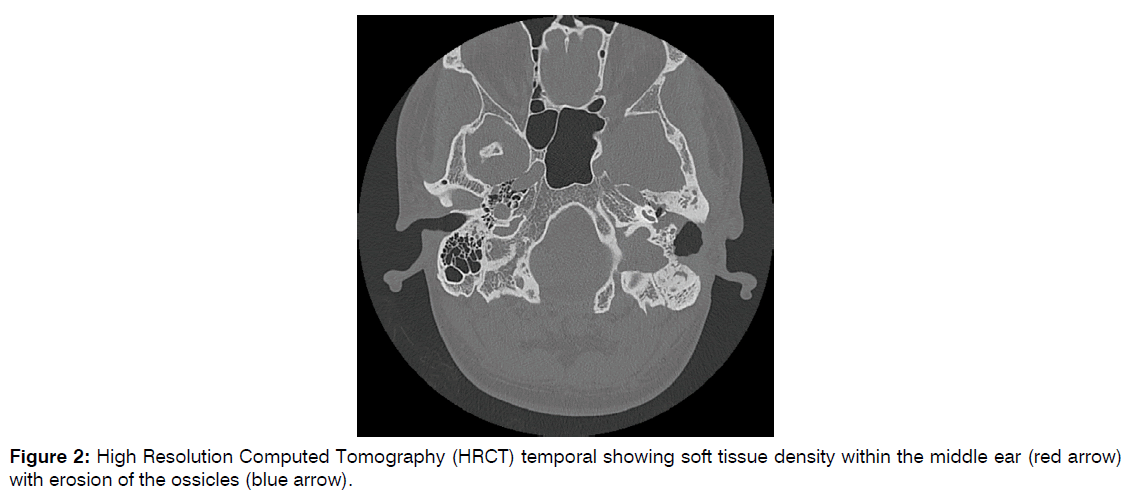
Figure 2: High Resolution Computed Tomography (HRCT) temporal showing soft tissue density within the middle ear (red arrow) with erosion of the ossicles (blue arrow).
High Resolution Computed Tomography (HRCT) temporal bone revealed soft tissue density within the middle ear with erosion of the ossicles and suggestive of recurrent left cholesteatoma.
Due to the above-mentioned findings, underwent left mastoid exploration in June 2018 for left recurrent cholesteatoma.
Intra operative findings revealed, cholesteatoma sac bulging from the poster superior part of TM. There was no pars flaccida perforation and no posterior wall sagging. There was cholesteatoma sac in the mastoid antrum, extending to epitympanum. Cholesteatoma pearl seen at the epitympanum then removed. There was presence of cholesterol granuloma in the middle ear.
The patient developed intermittent left ear discharge six weeks after surgery. Otoscopic findings showed granulation tissue covering the mastoid cavity. The patient was prescribed oral antibiotics and instructed to follow up in a month. Oral and topical antibiotics were used to treat the patient’s recurrent episodes of ear discharge that have since occurred on several occasions. Additionally, the patient did not com-ply with follow-ups during this time.
A repeat HRCT scan was recommended for the patient in January 2020, a year and a half after the redo surgery, due to recurrent ear discharge. Regretfully, the CT scan was not carried out because the patient neglected to follow up for eight months Figure 3.
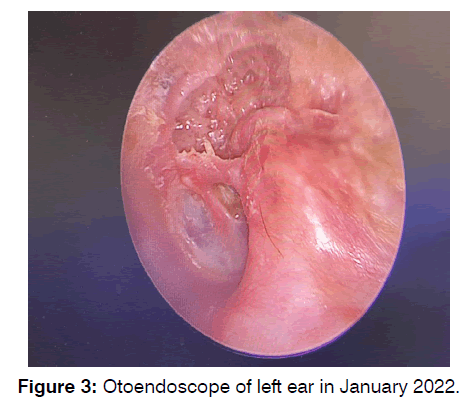
Figure 3: Otoendoscope of left ear in January 2022.
Discussion
Recurrent cholesteatoma remains the surgeon’s fear despite being in the antibiotic era and equipped with better visual aids and surgical instruments, even the most recent literature document the recurrence rate ranged from 13.2 to 22.1% in canal wall down surgeries [3]. A chronic discharging ear and cholesteatoma recidivism also have considerable bearing on the personal, emotional and social life of the patients, adversely affecting the qualityof- life factors.
A meta-analysis study by Tomlin et al. (2013) on the risk of cholesteatoma recidivism after Canal Wall Up (CWU) and Canal Wall Down (CWD) is of great importance. Authors reported a lower percentage of residual and recurrent disease after CWD (range 5% to 17%) compared to CWU surgery (range 9% to 70%) [4]. The significance of this case is that despite a thorough CWD surgery, patient developed recurrence of disease as early as 4 weeks.
Factors for development of recurrence of cholesteatoma in this case could be presence of recurrent infection of the ear. In this patient this can result from improper lifestyle modifications such as keeping the ear dry or untreated obstructive sleep apnea symptoms. A surgeon factor for development of recurrence could be incomplete surgical clearing. Megerian et al. (2002) outlined that the areas with persistent disease post-canal wall down surgery included sinodural angle (92%), tegmen cells (88%) and mastoid tip (62%), and implicated incomplete lowering of the facial ridge (94%) and inadequate meatoplasty (60%) [3].
Any redo surgery of the middle ear is challenging due to distorted anatomic land-marks and disease recrudescence. The aim of redo surgery are eradicating the causes of discharging ear, including recurrent cholesteatoma, and addressing the pitfalls of the primary surgeries, such as adequate lowering of facial ridge, complete removal of facial bridge, saucerization of the tympanomastoid cavity, truncating the mastoid tip region, cavity obliteration, and revising the meatoplasty as needed following cavity obliteration. Although lowering of facial ridge is fundamental process in CWD surgery it is more favorable for complete facial ridge removal in cases of cholesteatoma involving the sinus tympani, mesotympanum or supratubal recess [5]. In our case during redo surgery the facial ridge was brought down, and the cholesteatoma sac was removed.
Examination under general microscope is the single best method for detecting recurrent cholesteatoma. Otoendoscope is also another useful method in detecting recurrence by allowing illumination deep into the areas of interest. While performing revision canal wall down surgery, it is more favorable in terms of outcome using the endoscopic revision rather than microscope [6]. While to note that during our case microscopic revision surgery was performed the difference in superiority in terms of outcome for these two surgical techniques requires further study.
Computed Tomographic (CT) scan can be helpful also be valuable in diagnosing recurrent cholesteatoma. In the case of prior canal wall down mastoidectomy, CT shows the remaining bony anatomy and possible shortcomings of prior surgery, such as a high facial ridge and retained mastoid. High Resolution Computed Tomography (HRCT) had a sensitivity of 83.3% and specificity of 58.3% in detection of cholesteatoma, while Magnetic Resonance Imaging (MRI) has 91.6% accuracy in detecting cholesteatoma [7]. It was noted that the HRCT findings were 100% sensitive in predicting inadequately removed facial bridge and dehiscence of the lateral semicircular canal and were >80% sensitive in determining the presence of ossicles and bony overhang. It was found to be less satisfactory for predicting breaches in the tegmen and sinus plates, presence of high facial ridge and fallopian canal dehiscence. However, cholesteatoma appears as a soft tissue density on CT scan and thus may be indistinguishable from inflamed mucosa, granulation tissue, or retained fluid. The use of Magnetic Resonance Imaging (MRI) in conjunction with Computed Tomography has been advocated by some as the means of establishing or disproving recurrence. Diffusion-weighted MRI is another modality for detecting recurrent cholesteatoma3. It is shown that Diffuse Weighted Imaging (DWI) has excellent specificity that reduces the need for second look surgery. However, the drawback is that it still could not detect lesions smaller than 4mm.
The commonest reason for frequent visits to otolaryngologists following Canal Wall Down (CWD) procedures is intractable ear discharge due to keratin accumulation and granulation tissues that require repeated cavity care. Therefore, even though all cholesteatoma has been cleared, patient could still present with intermittent ear dis-charge.
According to a retrospective study done in University Kebangsaan Malaysia by Ab-dullah et. al (2013), dry ear was achieved in 78% of patients with 3% recurrence rate post CWD surgery [8]. Therefore, post Canal Wall Down (CWD) procedure, it is necessary for regular hospital follow-up visits for earwax removal and cleaning due to possible cavity infection and recurrence check-ups and lifestyle adjustments. In our case, one of the patient factors for development of recurrence could be non-compliance in follow up and evidence of major gap in of one and half years post first surgery. Most importantly, the need for revision surgery becomes evident when such a chronic draining cavity refuses to heal despite optimal medical management for a given period (an arbitrary period of a minimum of six months was considered). There is no consensus regarding the appropriate duration for follow-up following cholesteatoma surgery. Nearly 90% of recurrent disease cases can be detected within 5 years after surgery and for recidivism was 10.4 years [9]. Therefore, proper pre-operative patient counseling emphasizing of the long term follow up post-surgery is of utmost important.
Conclusion
We report a case of recurrent cholesteatoma despite canal wall down procedure requiring a second redo procedure and with persistent recurrent otorrhea after the redo procedure. Currently, patient’s ear is dry and do not show any evidence of recurrence cholesteatoma.
However, this case demonstrates the need for regular follow ups even after a canal wall down procedure for detecting recurrence of disease. Moreover, this case denotes some of the patient factors and surgeon factors involved in disease recurrence Furthermore, importance of opting for an imaging study in case of high suspicions of the disease.
References
- Smouha, Eric E., Bojrab, Dennis I. Cholesteatoma. Eur. Arch. Oto-Rhino-L. 2012; 269(4).
- Das S, Dutta M, Panja T, Sinha R. Chronic draining ear and cholesteatoma recidivism: a retrospection from clinical, imaging, and surgical perspectives.Turk Arch Otorhinolaryngol. 2019;57(3):133.
- Medany MM, Sabra RM, Hakim EK, Elshafei AM, Sadawy AM. Reliability of Diffusion Weighted MRI for the Diagnosis of Residual and Recurrent Cholesteatoma. Egypt J Hosp Med. 2018;72(10):5403-8.
- Bovi C, Luchena A, Bivona R, Borsetto D, Creber N, Danesi G. Recurrence in cholesteatoma surgery: what have we learnt and where are we going? A narrative review. ACTA Otorhinolaryngologica Italica. 2023;43(2):S48.
- Capriotti V, Dal Cin E, Gatto A, Rizzo PB, Danesi G, Tirelli G. Facial ridge management in canal wall down tympanoplasty for middle ear cholesteatoma. J Laryngol Otol. 2022:1-22.
- Binti Abdullah A, Hashim SM, Awang MA, Saim L. Outcome of canal wall down mastoidectomy: experience in sixty three cases. Med J Malays. 2013;68(3):217-21.
- Rao S. Role and utility of HRCT and MRI in detection and evaluation of cholesteatoma.
- Fermi M, Siggemann T, Melchiorri C, Bonali M, Niederhauser L, Caversaccio M, et al. Revision canal-wall down surgery: comparison of surgical outcomes with three different techniques. Eur Arch Oto-Rhino-L. 2022;279(4):1731-9.
- Kuo CL, Shiao AS, Yung M, Sakagami M, Sudhoff H, Wang CH, et al. Updates and knowledge gaps in cholesteatoma research. Bio Med Research International. 2015.
1Department of Otorhinolaryngology, Head and Neck Surgery, Faculty of Medicine, Universiti Kebangsaan, Malaysia, Kuala Lumpur
2Department of Radiology, Faculty of Medicine, Universiti Kebangsaan, Malaysia, Kuala Lumpur
3Centre of Hearing and Speech (Pusat-HEARS), Universiti Kebangsaan, Malaysia, Kuala Lumpur
Send correspondence to:
Fathmath Shana Mohamed
Department of Otorhinolaryngology, Head and neck surgery, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia, E-mail: fathmathshana1991@gmail.com
Tel: +60176461067
Paper submitted on November 17, 2023; and Accepted on December 08, 2023
Citation: Mohamed SF. Recurrent Cholesteatoma: Why it occurs?. Int Tinnitus J. 2023;27(2):242-246.


