The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 26, Issue 1 / June 2022
Original Paper Pages:57-62
10.5935/0946-5448.20220008
Ten Years Follow Up of Patients with Tinnitus and Normal Hearing
Authors: Helga Moura Kehrle, Ronaldo Campos Granjeiro, Andre Luiz L Sampaio, Carlos Augusto C P de Oliveira, Maria Stella de Farias, Vaneli Silva Martins
PDF
Abstract
Objective: To describe the natural history of tinnitus in normal hearing patients.
Study Design: This is a prospective longitudinal observational study.
Setting: Tertiary University Hospital.
Methods: In 2009 we studied 68 patients with significant tinnitus and normal hearing (Study Group-SG) compared to 46 patients with normal hearing and no tinnitus (Control Group-CG). We have been able to contact and recruit 24 patients from SG (35.3 %) and ten patients from CG) (21.74%) in 2019. Both groups were submitted to conventional audiometry, Distortion Product Otoacoustic Emissions (DPOAE), Tinnitus Handicap Inventory (THI), Visual Analog Scale (VAS) and Beck`S Depression and Anxiety Scales (BDS, BAS). These measures were compared with the same ones performed ten years ago in the same groups of patients. The software SPSS for windows version 21 was used. P values <0.05 were considered significant. Student t test was used to compare SG and CG results in 2019 and to compare 2009 and 2019 outcomes.
Results: Hearing loss, especially in the higher frequencies, were significantly worse in SG compared to GC in 2019. DPOAE were significantly worse in SG and CG in 2019 however CG had more abnormal results than SG. These results suggest that outer hair cells lesions are not the only determinant for tinnitus and hearing loss development.
Conclusions: These results suggest that outer hair cells lesions are not the only determinant for tinnitus and hearing loss development
Keywords: Tinnitus, Hearing loss, Longitudinal study.
Introduction
In 2009 we studied a group of 68 patients with significant tinnitus and normal hearing between 250 to 8000Hz. We compared this Study Group (SG) with a Control Group (CG) composed of 46 patients with normal hearing in the same frequencies, and no tinnitus.
Otoacoustic emissions [1] and auditory brainstem responses [2] were used to study the electrophysiology of tinnitus in normal hearing patients. Tinnitus Handicap Inventory (THI) Visual Analog Scale (VAS) the Beck’s Depression Inventory (BDI) and Beck’s Anxiety Inventory (BAI) were used to test the correlation between tinnitus annoyance and depression-anxiety disorders [2,3]. Both groups had normal hearing between 250 and 8000Hz.
The correlation of tinnitus with abnormal Distortion Product Otoacoustic Emissions (DPOAE) results was demonstrated in SG [1]. Although the averages obtained in the ABR results from the patients with and without tinnitus and normal hearing were within normal limits, tinnitus group presented a significant prolongation of the latencies and some interpeaks, suggesting that ABR might contribute to the workup of these patients [2]. Correlation of tinnitus with depression and anxiety was also documented [3,4].
In 2019 we were able to contact 24 patients from the SG and 10 individuals who were part of the CG in 2009. We decided to submit these patients to the same tests and questionnaires employed in the first project, compare the 2 groups (SG/CG 2019) and then compare these results with the ones obtained 10 years ago.
In this way we would describe the natural history of tinnitus in normal hearing patients along a ten years’ time interval. This communication describes the results of this project.
Method
The study was conducted at the Unit of the Institute of Strategic Management of the Federal District (IGES-DF), Brasilia-DF, Brazil. It was approved by the Research Ethics Committee of that Institution, under approval number 16205019.2.0000.8153, and with the signature of the Free Research Informed Consent Form by the participants.
The SG in 2009 was composed of 68 patients, who had significant tinnitus and normal hearing from 250 to 8000HZ. Individuals with tinnitus and hearing loss or with otological diseases were excluded. At the time, CG was composed of 46 patients with no tinnitus and normal hearing. Both groups were comparable regarding age and sex.
In 2019 we were able to contact 24 (35.3%) patients from the original SG and 10 (21.7%) patients from the original CG. As in the previous 2009 study, none of the patients in the current sample had somatosensorial tinnitus, middle ear disease or tympanic membrane perforation.
All patients from both groups were submitted to tonal and vocal audiometry and Distortion Product Otoacoustic Emissions (DPOAE) tests. Tinnitus annoyance was quantified using Visual Analog Scale (VAS) and Tinnitus Handicap Inventory (THI) questionnaire. Level of Depression and Anxiety were measured by Beck`s Depression and Anxiety Inventories (BDI and BAI).
SG and CG results were compared in 2019 the same way they had been compared 10 years ago. In addition, the 2019 results were compared with 2009 results and the significances of the differences were verified.
PSS software version 21 for windows was employed for statistical analysis. In order to compare DPOAE median results with the THI scores presented by categories between SG and CG Student`s T Test was used.
In order to compare the 2019 results with the ones from 10 years ago the median differences between them in each exam were tested using the Student`s T Test. Chi-squared test was employed to verify associations between categorical variables and results of THI, BDI and BAI presented as categories.
Results
In 2009 the SG had 68 patients with tinnitus and normal hearing. CG was composed of 46 patients with normal hearing and no tinnitus. In 2019 SG consisted of 24 patients who were part of SG in 2009. The CG in 2019 involved 10 patients from the original CG group of 2009 (Table 1).
| Pacients | Control Group (CG) | Study Group (SG) | |||
|---|---|---|---|---|---|
| 2009 | 2019 | 2009 | 2019 | ||
| By age | N | 10 | 10 | 24 | 24 |
| Mean | 33.6 years | 42.5 years | 37.5 years | 47.2 years | |
| Minimum | 29.0 years | 38.0 years | 17.0 years | 28.0 years | |
| Maximum | 43.0 years | 52.0 years | 46.0 years | 54.0 years | |
| By sex | N | 10 | 10 | 24 | 24 |
| Female | 5 | 5 | 12 | 12 | |
| Male | 5 | 5 | 12 | 12 | |
Table 1: Number of participants in the years 2009 and 2019 in the SG and CG according to age and sex.
Regarding the location of the tinnitus symptom (left ear, right ear or in the head), 17 patients (70.8%) continued to report the symptom in the same location as in 2009 and six patients (25%) underwent changes during the past 10 years. In 2009, 62.5% had tinnitus in both ears, 8.3% in the head, 4.2% in the right ear and 25% in the left ear. In 2019, one of the patients tested had tinnitus resolution, 70.8% had tinnitus in both ears, 8.3% in the head and 16.7% of the patients referred tinnitus in the left ear. In the current sample, no patient had tinnitus in the right ear.
There were no significant differences between SG and CG regarding age and sex neither in 2009 nor in 2019.
Table 2 shows that there were no significant variations in tinnitus annoyance measured by VAS between the 2009 and the 2019 SG. One patient in SG reported that tinnitus was no longer present. None of the ten patients in CG had developed tinnitus in ten years.
| Tinnitus Characterization | STUDY GROUP (SG) | P value | ||
|---|---|---|---|---|
| 2009 | 2019 | |||
| Intensity | Mean | 4.7 | 4.5 | 0.682 |
| Standard deviation | 2.1 | 2.1 | ||
| Annoyance | Mean | 4.3 | 3.8 | 0.461 |
| Standard deviation | 2.7 | 3.4 | ||
| Impact | Mean | 2.8 | 2.8 | 1,000 |
| Standard deviation | 2.6 | 2.7 | ||
Table 2: Difference between tinnitus intensity, annoyance and impact in the period between 2009 to 2019 according to VAS.
When we measured tinnitus annoyance using THI no significant differences were found between the 2009 and the 2019 study. In other words, the symptom had not progressed nor regressed significantly during ten years follow up.
Correlation of anxiety measured by BAI and tinnitus annoyance measured by THI was non-significant in 2009 (p=0.086) but was significant in 2019 (p=0.005).
Correlation of depression measured by BDI, and tinnitus annoyance measured by THI were significant both in 2009 (p=0.03) as in 2019 (p=0.029).
When we looked at the variation of anxiety and depression scores between 2009 and 2019, we found that anxiety scores varied markedly from one point to the other. Depression scores also varied but less than the anxiety ones. (BAI scores-SG-10.2 -CG-2.2 in 2009; SG-9.6; CG 5.8 in 2019).
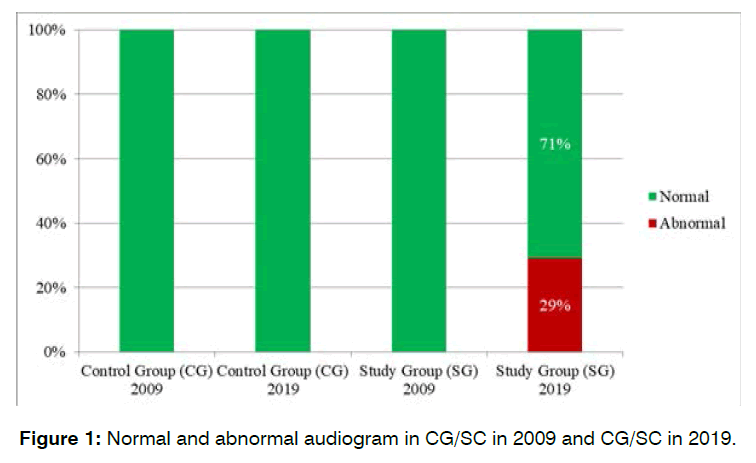
In 2009, both SG and CG were composed of only normal hearing patients. Analysis of audiometric results in 2019 showed that in the SG of 24 patients recruited (48 ears), 70.2% of the ears had normal hearing results and 29,2% of the ears had progressed to some degree of hearing loss (Figure I). CG had 100% of ears maintained the normal hearing results after 10 years. The difference between SG and CG was statistically significant (p<0.05).
Figure 1: Normal and abnormal audiogram in CG/SC in 2009 and CG/SC in 2019.
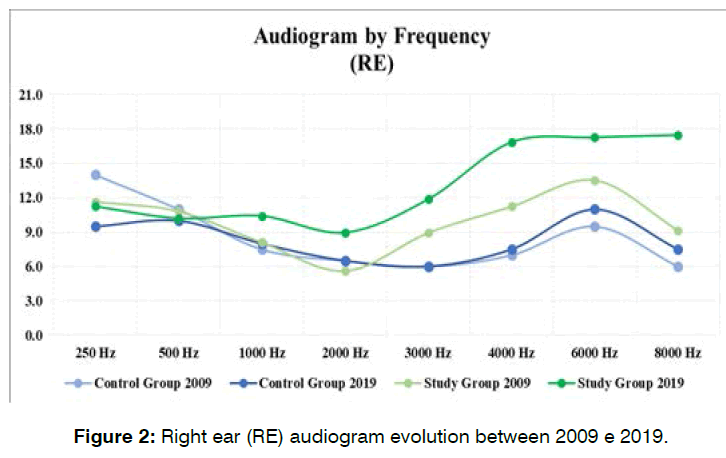
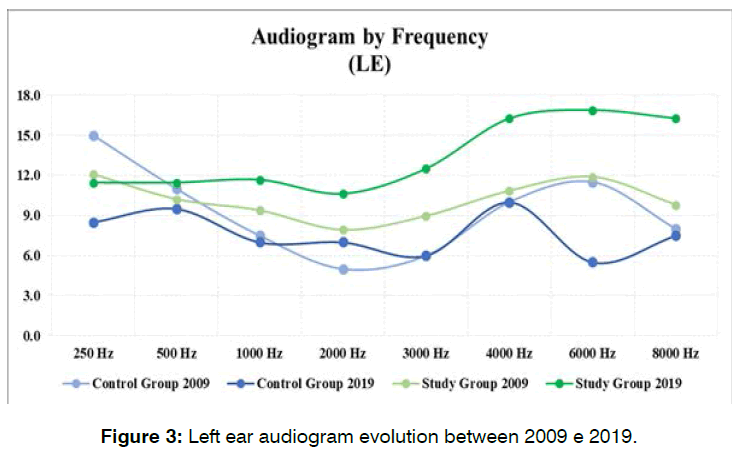
Differences between SG and CG audiometric results in 2009 and 2019 analyzed by frequencies and by side are showed in Figures 2 and 3. In SG there were significant differences in 1000Hz (p=0.038), 4000Hz (p=0.01) and 8000Hz (p=0.003) in the right ears and in 4000Hz (p=0.006), 6000Hz (p=0.035) and in 8000Hz (p=0.18) in the left ear. In CG there were no differences in the right ears but in the left ear, although all frequencies parameters were within normal limits, we observed differences in 250Hz (p= 0.009) and 6000Hz (p=0.03).
Figure 2: Right ear (RE) audiogram evolution between 2009 e 2019.
Figure 3: Left ear audiogram evolution between 2009 e 2019.
Analysis of DPOAE results in SG and CG in 2009 and 2019 are showed in Table 3. In 2009 the SG had 23 ears (47.9%) with abnormal results, in 2019, the SG had 35 ears (72%) with altered results. This difference was statistically significant (P=0.012).
| DPOAE Evolution |
CG 2009 | CG 2019 | SG 2009 | SG 2019 |
|---|---|---|---|---|
| Abnormal | 15.0% | 85.0% | 47.9% | 72.9% |
| Normal | 85.0% | 15.0% | 52.1% | 27.1% |
| Total | 100.0% | 100.0% | 100.0% | 100.0% |
Table 3: Normal and altered DPOAE in the Control Group (CG) and Study Group (SG) between the years 2009 and 2019.
The CG had 3 ears (15%) with abnormal results in 2009 and 17 ears (85%) with affected results in 2019. This difference was also statistically significant (p=0.005).
Description of DPOAE evolution from 2009 to 2019 is showed in Table 3. The greatest frequency of abnormal results in SG and CG was found in 8000Hz.
Discussion
This is a prospective longitudinal study that evaluates part of the same group of patients with tinnitus and normal hearing at two different times, 2009 and 2019, an interval of 10 years. We know that when placed in a soundproof booth 94% of randomly chosen people will notice tinnitus but as a transient symptom [4]. In turn, in this study the tinnitus symptom was important enough to motivate the patients to seek medical advice.
In 2009, we found more abnormal DPOAE results in normal hearing patients with tinnitus (SG) when compared with normal hearing people without tinnitus (CG) [1], so, we concluded that outer hair cells lesions were probably the starting point of tinnitus. In another study, Brainstem auditory responses also showed clear differences between patients with (SG) and without (CG) tinnitus and normal hearing, although within normal limits, tinnitus group presented a significant prolongation of the latencies and some interpeaks, suggesting that ABR might contribute to the evaluation of these patients [2]. The same authors demonstrated in another research, a positive correlation between DPOAE results, annoyance of tinnitus and levels of anxiety and depression in normalhearing patients with tinnitus [3].
In 2019 we were able to recruit only 24 of the 68 original patients from the original SG of 2009 and 10 of the original 46 patients of CG. Brasília usually receives many patients from out of state and most do not have the financial means to travel frequently for medical appointments, when they get a cost allowance from the government, which involves a lot of bureaucracy and available funds. Some changed address and phone numbers and were not reachable. This was the main reason our SG and CG were much smaller in the present study.
We decided to submit these groups of patients to the same protocol we used in 2009 trying to answer the questions: what happened to tinnitus in SG during a ten years’ time? Did any of the CG participants develop tinnitus? What happened to the hearing level of the participants in the SG and CG?
No one in the CG developed tinnitus from 2009 to 2019. One patient in the SG stated tinnitus was no longer present. Tinnitus annoyance measured by THI did not change significantly during ten years follow up. Depression and anxiety have been shown to commonly accompany tinnitus [5,6], correlating moderately with tinnitus-related distress [7] Correlation of THI results with BAS results were negative in 2009 and positive ten years later. THI results and BDS scores were positively correlated both in 2009 and 2019. Levels of anxiety varied much more between 2009 and 2019 than those of depression. In 2019 29.2% of SG patients had sensorineural hearing loss while CG patients had normal hearing. DPOAE tests results were worse in 2019 than in 2009 in both SG and GC patients. CG had slightly worse results than SG.
There is one answer from the above results: patients with tinnitus ten years ago developed hearing loss during this period, but not patients without the symptom. This seems to indicate tinnitus might predict a hearing loss. The fact that DPOAE results in both groups were much worse in 2019 than in 2009, seems to indicate that DPOAE results are not related to hearing loss neither to tinnitus.
According to Nondahl et al [8], most tinnitus cases are associated with some degree of hearing loss (67.7%). Although different pathologies affecting hearing can be associated with tinnitus [9], the exact mechanisms behind how tinnitus and hearing loss remains unanswered.
Why did 2009 CG patients not develop tinnitus nor hearing loss even though the results of DPOAE were worse in CG than in SG ten years later? These results strengthen the notion that, outer hair cells lesion alone, may not always lead to tinnitus and/or hearing loss detected by standard pure tone audiograms. Other mechanisms are probably involved as well. As standard pure tone audiograms only sample at octave or inter-octaves and do not test higher frequencies, they potentially can miss lesions between the tested frequencies or frequencies above 8000Hz.
In this study, the presence of tinnitus appears to predict incoming hearing loss in some cases. However, patients certainly can develop hearing loss without having tinnitus. Again, the presence of tinnitus as a predictor of hearing loss probably depends on the sensitivity of central pathways. More studies are needed.
These findings agree with Jastreboff’s theory proposed in 1990. Tinnitus starts in the cochlea and is modified in the central pathways where it can become a very intense and disturbing symptom associated with emotional and autonomic pathways [10].
Hearing loss does not seem to be related to outer hair cells lesions alone, for in the present study, DPOAE results in 2019 were slightly worse in CG compared to SG. In a temporal bone research, Oliveira, Schuknecht and Glynn [11] found that the majority of temporal bones of patients who complained of significant tinnitus during life had normal histology. Unfortunately, the audiograms of these patients were not studied.
Recently Viana et al [12] showed that synaptic changes precede lesions of the organ of Corti and explains sensorineural hearing loss in the absence of inner hair cells lesions (hidden hearing loss). This may be the case here.
Standard pure tone audiograms only sample at octave or inter-octaves, so they can miss lesions between two tested frequencies. Xion et al [13] using fine frequency resolution (1/24 octave step) audiometry, referred as precision pure tone audiogram, confirmed hidden cochlear impairments in tinnitus patients with apparently normal audiograms.
A more comprehensive hearing assessment would benefit tinnitus studies, providing higher sensitivity for auditory system impairments [13-15].
There are limitations of this work that must be addressed: High frequency audiometry (above 8000Hz) was not performed because it was not available to us in 2009. It is now well known that patients with tinnitus usually have hearing loss when these higher frequencies are tested [14-18]. This test would probably enhance our results.
There was a large loss from 68 to 24 patients in SG from 2009 to 2019. These 24 patients were the ones we were able to contact, as explained earlier. In other words, they were not selected, but randomly picked up. As the SG in 2009 was homogenous regarding age and sex we believe these 24 patients do represent the original group. Also, we were able to contact only 10 of the 46 original patients from the 2009 CG. As a voluntary control group, many were not willing to go to the hospital for the tests, claiming that they did not have time, even after being informed about the relevance for the study. This group was also homogenous as far as age and sex were concerned, and they were all healthy. Both groups were composed of middle-aged adults and tinnitus annoyance in SG was predominantly mild to moderate (VAS 5 to 7), enough to induce the patients to search for medical attention.
Because of the small size of the samples, parametric tests could not be appropriate for the statistical analysis. We therefore also ran paired tests to see if the results would be different. Paired tests results were no different from the ones obtained with the parametric tests (data not shown). A recent review19 brings together relevant studies about tinnitus, covering from its generation mechanisms, epidemiology, evaluation, and treatment development, aiming to highlight the main challenges and provide suggestions for further research. One of the obstacles in understanding and unveiling tinnitus is the difficulty of achieving studies with a larger number of patients.
Conclusion
Twenty nine percent of SG patients progressed to some degree of sensorineural hearing loss in 2019 but all patients in CG maintained normal hearing at the 10 years follow-up. These results suggest that tinnitus could predict hearing loss in higher frequencies, not reached in conventional audiometry. Perhaps if high-frequency audiometry above 8000Hz) had been performed in the 2009 study, they would already be abnormal at that time. We know from literature that tinnitus patients usually have sensorineural hearing loss in the higher frequencies. It follows that the origins of sensorineural hearing loss and tinnitus are very closely related.
DPOAE showed significantly more abnormal results in SG than in CG in 2009. In 2019 the incidence of DPOAE abnormalities was no different in SG and CG but this fact did not influence tinnitus and hearing loss. These results suggest that outer hair cells lesions are not the only determinant for tinnitus and hearing loss development.
Inner hair cells and their synapses should be looked upon in the future (hidden hearing loss in search of the cochlear trigger of tinnitus.
Our results must be confirmed by prospective studies involving larger samples because of the shortcomings discussed above.
References
- Granjeiro RC, Kehrle HM, Bezerra RL, Almeida VF, André LS, Oliveira CA. Transient and distortion product evoked oto-acoustic emissions in normal hearing patients with and without tinnitus. Otolaryngol—Head and Neck Surg. 2008;138(4):502-6.
- Kehrle HM, Granjeiro RC, Sampaio AL, Bezerra R, Almeida VF, Oliveira CA. Comparison of auditory brainstem response results in normal-hearing patients with and without tinnitus. Arch of Otolaryngol–Head & Neck Surg. 2008;134(6):647-51.
- Campos Granjeiro R, Moura Kehrle H, Sarmento Cardoso de Oliveira T, Lopes Sampaio AL, Costa Pires de Oliveira CA. Is the degree of discomfort caused by tinnitus in normal-hearing individuals correlated with psychiatric disorders?. Otolaryngol--Head and Neck Surg. 2013;148(4):658-63.
- Heller MF, Bergman M. Tinnitus aurium in normal hearing persons. Ann Otol Rhinol & laryngol. 1953; 62:73-82.
- Stobik C, Weber RK, Münte TF, Walter M, Frommer J. Evidence of psychosomatic influences in compensated and decompensated tinnitus: evidencia de influencias psicosomáticas en acúfenos compensados y descompensados. Int J Audiol. 2005;44(6):370-8.
- Udupi VA, Uppunda AK, Mohan KM, Alex J, Mahendra MH. The relationship of perceived severity of tinnitus with depression, anxiety, hearing status, age and gender in individuals with tinnitus. The Int Tinnitus J. 2013;18(1):29-34.
- Langguth B, Landgrebe M, Kleinjung T, Sand GP, Hajak G. Tinnitus and depression. The World J Biol Psyc. 2011;12(7):489-500.
- Nondahl DM, Cruickshanks KJ, Wiley TL, Klein R, Klein BE, Tweed TS. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. J Am Acad of Audiol. 2002;13(06):323-31.
- Baguley D, McFerran D, Hall D. Tinnitus. The Lancet. 2013;382(9904):1600-7.
- Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990;8(4):221-54.
- Oliveira CA, Schuknecht HF, Glynn RJ. In search of cochlear morphologic correlates for tinnitus. Arch of Otolaryngol–Head & Neck Surg. 1990;116(8):937-9.
- Viana LM, O'Malley JT, Burgess BJ, Jones DD, Oliveira CA, Santos F, et al. Cochlear neuropathy in human presbycusis: Confocal analysis of hidden hearing loss in post-mortem tissue. Hearing Res. 2015;327:78-88.
- Xiong B, Liu Z, Liu Q, Peng Y, Wu H, Lin Y, Zhao X, Sun W. Missed hearing loss in tinnitus patients with normal audiograms. Hearing Res. 2019;384:107826.
- Vielsmeier V, Lehner A, Strutz J, Steffens T, Kreuzer PM, Schecklmann M, et al. The relevance of the high frequency audiometry in tinnitus patients with normal hearing in conventional pure-tone audiometry. BioMed Res Int. 2015.
- Lefeuvre J, Chedeau J, Boulet M, Fain G, Papon JF, Nguyen Y, et al. Hidden hearing loss and tinnitus: utility of the high-definition audiograms in diagnosis. Clinical otolaryngol: official J ENT-UK; official J Netherlands Soci for Oto-Rhino-Laryngol & Cervico-Facial Surg. 2019;44(6):1170-5.
- Ukaegbe O, Ezeanolue B, Orji F. The influence of tinnitus on the audiometric threshold of sufferers. Int Arch of Otorhinolaryngol. 2016;20:339-43.
- Sanchez TG, Mak MP, Pedalini ME, Levy CP, Bento RF. Tinnitus and hearing evolution in normal hearing patients. Int Arch Otorhinolaryngol. 2005;9(3):220-7.
- Yildirim G, Berkiten G, Kuzdere M, Ugras H. High frequency audiometry in patients presenting with tinnitus. The J Int AdvOtol. 2010;6(3):401.
- Simoes JP, Daoud E, Shabbir M, Liyanage N, Riha C. Corrigendum: Multidisciplinary Tinnitus Research: Challenges and Future Directions From the Perspective of Early Stage Researchers. Frontiers in Aging Neurosci. 2021;13:730758.
1Professor of Otolaryngology- Instituto de Gestão Estratégica de Saúde Do Distrito Federal Brasília-DF, Brasil.
2Professor of Otolaryngology- Brasília University Medical School (UNB). Brasília-DF, Brasil.
3Third year Medical Resident in Otolaryngology - Instituto de Gestão Estratégica de Saúde Do Distrito Federal, Brasília-DF, Brasil
Send correspondence to:
Helga Moura Kehrle
Professor of Otolaryngology- Instituto de Gestão Estratégica de Saúde Do Distrito Federal Brasília-DF, Brasil, E-mail: helgak1@hotmail.com
Paper submitted on March 25, 2022; and Accepted on May 02, 2022
Citation: Helga Moura Kehrle, Ronaldo Campos Granjeiro, Andre Luiz L Sampaio, Carlos Augusto C P de Oliveira, Maria Stella de Farias, Vaneli Silva Martins. Ten Years Follow Up of Patients with Tinnitus and Normal Hearing. Int Tinnitus J. 2022;26(1):57-62.