The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 27, Issue 2 / December 2023
Research Article Pages:174-182
10.5935/0946-5448.20230027
The Effect of Clonidine Premedication on Hemodynamic Changes Following Tracheal Intubation and Co2 Gas Insufflation and Postoperative Shivering In Patients Undergoing Laparoscopic Cholecystectomy; a Randomized Clinical Trial
Authors: Masood Entezariasl, Khatereh Isazadehfar*, Maryam Raesi
PDF
Abstract
Background: Laparoscopic cholecystectomy is a proper treatment for cholecystitis but the Carbon dioxide gas which is used in surgery stimulates the sympathetic system and causes hemodynamic changes and postoperative shivering in patients undergoing operations. This study was conducted to evaluate the effects of clonidine on reducing hemodynamic changes during tracheal intubation and Carbon dioxide gas insufflation and postoperative shivering in patients undergoing laparoscopic cholecystectomy. Material and Methods: This prospective, randomized, triple-blind clinical trial was conducted on 60 patients between the 18-70 years-old age group, who were candidates of laparoscopic cholecystectomy surgery. The patients randomized into two groups (30 patients received 150 μg oral clonidine) and 30 patients received 100 mg oral Vitamin C). Heart rate and mean arterial pressure of patients were recorded before anesthesia, before and after laryngoscopy, before and after Carbon dioxide gas insufflation. Data were analyzed using Chi-2, student t-test, and analysis of variance by repeated measure considering at a significant level less than 0.05. Results: The findings of this study showed that both heart rate and mean arterial pressure in clonidine group after tracheal intubation and Carbon dioxide gas insufflation were lower than patients in the placebo group, but there was not any statistically significant difference between the two groups (p>0.05) and also postoperative shivering was not different in groups. There was no significant statistical difference in postoperative shivering between the two groups (p>0.05). Conclusion: Using 150 μg oral clonidine as a cheap and affordable premedication in patients undergoing laparoscopic cholecystectomy improves hemodynamic stability during operation.
Keywords: Intubations; Pneumoperitoneum; Clonidine; laparoscopy; homodynamic.
Introduction
Laparoscopic surgery as a modern surgical technique has become very popular in common abdominal surgery such as cholecystectomy. The first laparoscopic cholecystectomy was done by Philippe Mort in 1987. The advantages of laparoscopic surgery compared to the open surgeries include reduced pain for smaller incisions, less blood loss, shorter recovery time, and faster return to normal life. The key element in laparoscopic surgery is forming pneumoperitoneum which is mostly provided by CO2. Major problems during laparoscopic surgery are related to CO2-induced pneumoperitoneum, which can affect the cardiopulmonary function and cause systemic absorption of carbon dioxide, extra-peritoneal insufflation, and intravenous gas embolism, Intra-abdominal organ injury, hemodynamic disorders due to decreased cardiac output, increased systemic vascular resistance, and increased pulmonary vascular resistance. These physiological effects of CO2 gas are caused by two different mechanisms, including the mechanical effects of increased intra-abdominal pressure and the chemical effects of CO2 gas [1,2].
Various strategies have been used to reduce these pneumoperitoneum-induced hemodynamic changes that make laparoscopic cholecystectomy safer for patients. Using drugs such as nitroglycerin [3] α-2 agonists such as clonidine [4], esmolol, magnesium sulfate, is one of these strategies which has been associated with some successes and practical limitations [5].
Laryngoscopy and endotracheal intubation during the general anesthesia, are accompanied by hemodynamic changes such as tachycardia, hypertension, a wide range of arrhythmias, and myocardial ischemia. These changes take place immediately after laryngoscopy and endotracheal intubation. Stimulation of the larynx following laryngoscopy increases plasma norepinephrine level by increasing sympathetic activity [6].
Clonidine is a α-2 adrenergic receptor agonist with a halflife of 9 to 12 hours, which is rapidly and completely been absorbed after oral administration and reaches a peak plasma concentration within 60 to 90 minutes. Clonidine has central sympatholytic effects, anesthesia, sedation, and pain relief. As a pretreatment for anesthesia, it slows the increase in hormonal responses such as catecholamine, cortisol, and vasopressin release during surgery. Reduces cardiovascular response and surgical stress and prevents the increase in heart rate and mean arterial pressure. It also increases the sensitivity of the cardiac baroreceptor reflex to the increase in systolic blood pressure, thereby stabilizing blood pressure [7].
Shivering after surgery is a common complication that is seen in about 55% of patients in recovery [8], which often occurs due to central hypothermia and vascular contraction in the body [9]. This physiological response may lead to much physiological impairment such as hypoxia, lactic acidosis, exacerbation of postoperative pain, increased oxygen consumption, carbon dioxide production, and increased intracerebral and intraocular pressure [8]. The best way to prevent of these side effects is the prevention of postoperative shivering and clonidine can prevent it by affecting on the central body temperature regulation system [9].
In this study, we investigated the hemodynamic stability during endotracheal intubation and pneumoperitoneum in laparoscopic cholecystectomy with oral clonidine compared with placebo. Postoperative shivering reduction was also considered as a secondary outcome.
Material and Methods
The present study was a triple-blind clinical trial conducted in Imam Khomeini Hospital of Ardabil in 2016-2017. Sixty patients with ASA class I, II and age range of 18-70 years-old who were candidates for elective Laparoscopic cholecystectomy under general anesthesia, were included in the study. Patients with a history of hypertension, morbid obesity, severe hepatitis, renal and endocrine dysfunction, cardiovascular disease, and patients who were dissatisfied with the study were excluded.
The patients underwent randomization and divided into two groups (30 patients in clonidine group (receiving 150 μg oral clonidine) and 30 patients in placebo group (receiving 100 mg oral Vitamin C). The group allocation was concealed using a random number generator, and the results placed into consecutively sealed numbered envelopes by a third party not involved in the trial. Neither patients, nor the researcher responsible for data collection, nor the analyzer were aware of the type of prescription drug.
The sample size was estimated based on study power of 80% and type I error of 5% and using the results of previous studies to obtain a statistically significant difference according to the following formula in each group of 30 people.
Thirty minutes before anesthesia, cardiopulmonary monitoring done for patients as a routine and ECG, Basic vital signs (mean arterial pressure, heart rate, and oxygen saturation), age, sex, and weight of all patients were recorded and according to randomization, patients received oral Clonidine 150 μg as Clonidine group or oral vitamin C 100 mg as placebo group.
Then the patients underwent general anesthesia in both the groups with fentanyl 2µg/kg and propofol 2mg/kg, and endotracheal intubation was performed by muscular relaxation with atracurium. 0.5 mg/kg. A combination of 50% oxygen, 50% N2O and 1-1.5% isoflurane were used to maintain anesthesia.
Pneumoperitoneum (PNP) was created by insufflation of CO2 into peritoneum (12mmHg Intra-Abdominal Pressure (IAP)), in supine position and then operation table was tilted to 10-15 degrees in reverse Trendelenburg position with left lateral tilt.
Patients were mechanically ventilated to keep End Tidal Carbon Dioxide (EtCO2) at 25-35 mmHg. During surgery, Ringer solution was administered in maintenance dose and any incidence of bradycardia (HR <50) was treated by atropine 0.5 mg I.V, any hypotension (MAP<20% preoperative) was treated with IV fluid bolus of Ringer lactate 250-300 ml. If hypotension did not respond to this management, 5mg intravenous bolus dose of ephedrine was administered.
At the end of surgery, the remaining neuromuscular block was reversed using an appropriate dose of neostigmine and atropine and after extubation the patient was transferred to the recovery room.
The study parameters including heart rate (HR beats/ minute), systolic blood pressure (SBP mmHg), diastolic blood pressure (DBP mmHg), and mean arterial pressure (MAP mmHg) were monitored and recorded at the following instances during the study period:
1- The basic vital signs
2- Before laryngoscopy
3- After tracheal intubation (in 1-5 min time interval)
4- Before CO2 insufflation
5- 5 min after CO2 insufflation
6- 10 min after CO2 insufflation
7- 15 min after CO2 insufflation
8- 30 min after CO2 insufflation
In recovery room patients were monitored for any evidence of complications or adverse effects. In addition, postoperative shivering was assessed and recorded as the secondary outcome based on muscular movement in recovery room.
Statistical analysis
Qualitative variables were reported as frequency, percentage, and quantitative variables were reported as mean and standard deviations. The results were analyzed using the descriptive statistical method and were presented as tables and figures, and analytical statistical methods using Chi-square test, Fisher’s exact test, T-test, and analysis of variance (ANOVA) with repeated measurements based on variable type, using SPSS (v.21) software. Significant level in all cases was considered to be less than 0.05.
Results
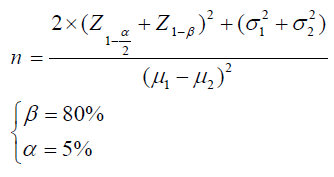
In this study, 60 patients were enrolled. No one was excluded during the assessment for eligibility and follow-up. Therefore, final analysis was done for all individuals Figure 1.
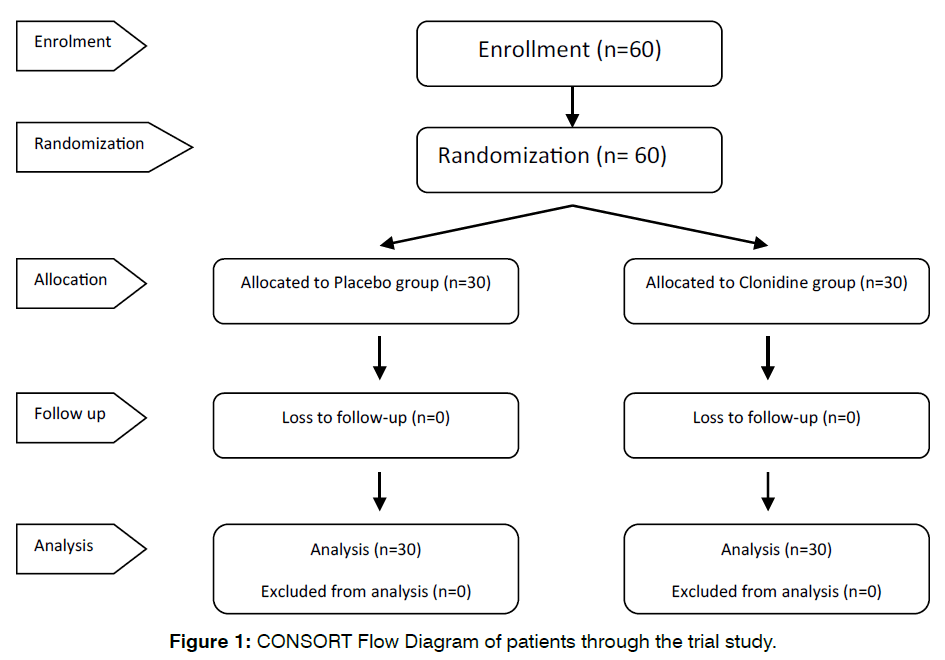
Figure 1: CONSORT Flow Diagram of patients through the trial study.
There was no significant difference between the groups with regard to demographic data such as age, sex, weight, height, duration of anesthesia, duration of surgery and preoperative vital parameters Table 1.
| Variable | Placebo (N=30) | Clonidine (N=30) | P value |
|---|---|---|---|
| Gender (M/F) | 3/27 | 6/24 | 0.47 |
| Age (year) | 44.17 ± 14.7 | 42.07 ± 14.24 | 0.57 |
| Weight (Kg) | 75.53 ± 18.69 | 71.38 ± 10.51 | 0.29 |
| Height (Cm) | 162.03 ± 8.03 | 160.03 ± 7.97 | 0.34 |
| Duration of surgery (min) | 48.17 ± 13.72 | 46.7 ± 12.53 | 0.67 |
| Duration of anesthesia (min) | 78.13 ± 19.44 | 71.87 ± 13.1 | 0.15 |
| Preoperative MAP (mmHg) | 107.8 ± 14 | 102.7 ± 13.7 | 0.19 |
| Preoperative HR (mmHg) | 85.3 ± 18.6 | 81.9 ± 14 | 0.44 |
Table 1: Demographic and baseline characteristics of the study population
Baseline vital parameters before induction (MAP and HR) in both the groups were comparable and not statistically significant as seen in Table 2 and 3.
| Heart Rate | Placebo (N=30) µ ± δ |
Clonidine (N=30) µ ± δ |
P-value+ |
|---|---|---|---|
| Baseline | 85.3 ± 18.6 | 81.9 ± 14 | 0.44 |
| Before Laryngoscopy | 77.2 ± 11.6 | 77 ± 14.2 | 0.95 |
| Immediately after Laryngoscopy | 83.6 ± 15.2 | 83.5 ± 13.4 | 0.97 |
| 1min after Laryngoscopy | 78.2 ± 15.6 | 81 ± 16.7 | 0.49 |
| 2 min after Laryngoscopy | 78.6 ± 19.3 | 78.9 ± 16.3 | 0.95 |
| 3 min after Laryngoscopy | 75.8 ± 17.8 | 76.9 ± 15.9 | 0.78 |
| 4 min after Laryngoscopy | 74.8 ± 16.5 | 76.7 ± 16.2 | 0.65 |
| 5 min after Laryngoscopy | 73.9 ± 15.1 | 76.7 ± 16.6 | 0.5 |
| Before CO2 Insufflation | 74.2 ± 16.1 | 75.9 ± 18.2 | 0.7 |
| 5 min after CO2 Insufflation | 76.6 ± 12.9 | 78.3 ± 17.5 | 0.68 |
| 10 min after CO2 Insufflation | 79.2 ± 11.9 | 79.6 ± 20 | 0.91 |
| 15 min after CO2 Insufflation | 79.4 ± 11.8 | 80.5 ± 19 | 0.8 |
| 30 min after CO2 Insufflation | 79.9 ± 13.1 | 80.5 ± 14.5 | 0.86 |
Table 2: Changes in heart rate in two groups at different study intervals
| Mean Arterial Pressure | Placebo (N=30) µ ± δ |
Clonidine (N=30) µ ± δ |
P-value |
|---|---|---|---|
| Baseline | 107.8 ± 16 | 102.7 ± 13.7 | 0.19 |
| Before Laryngoscopy | 81.4 ± 17.1 | 78.1 ± 15.2 | 0.44 |
| Immediately after Laryngoscopy | 100.7 ± 23.3 | 90.1 ± 16.9 | 0.049* |
| 1min after Laryngoscopy | 91.8 ± 16.2 | 86.9 ± 13.8 | 0.22 |
| 2min after Laryngoscopy | 93.2 ± 13.9 | 86.2 ± 14.5 | 0.06 |
| 3min after Laryngoscopy | 91.9 ± 18 | 85.5 ± 16.3 | 0.15 |
| 4min after Laryngoscopy | 91.6 ± 16.5 | 84.2 ± 16.7 | 0.08 |
| 5min after Laryngoscopy | 90.2 ± 15.9 | 86.7 ± 18.7 | 0.44 |
| Before CO2 Insufflation | 102.6 ± 16.9 | 93.8 ± 16.6 | 0.046* |
| 5min after CO2 Insufflation | 113.7 ± 17.1 | 103 ± 19.3 | 0.028 * |
| 10min after CO2 Insufflation | 106.6 ± 19.9 | 103.2 ± 15.7 | 0.47 |
| 15min after CO2 Insufflation | 101 ± 14.4 | 103.4 ± 13.5 | 0.51 |
| 30min after CO2 Insufflation | 98.3 ± 13.7 | 103.3 ± 14.9 | 0.18 |
Table 3: Changes in Mean Arterial Pressure in two groups at different study intervals
Heart rate after laryngoscopy was higher in clonidine group than the placebo group in all time sections, but this difference was not statistically significant (within group: F(12, 696) = 0.39 p=0.86) Table 2.
The effect of time based on the changes of the mean heart rates of patients was significant in both groups (within group: F (12, 696) = 4.9 p<0.001) Figure 2.
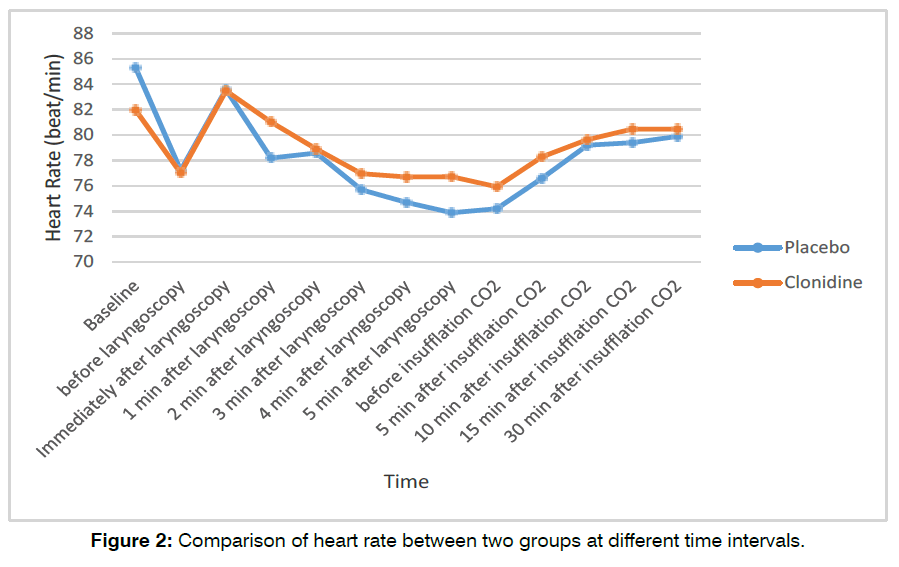
Figure 2: Comparison of heart rate between two groups at different time intervals.
The mean heart rate of patients in the time interval before and after laryngoscopy in both groups had significant difference (p <0.001 and F (1, 58) = 16.98), (but the mean of these changes were not significant in both groups), (p =0.974 and F (1, 58) = 0.001) and increased with the same ratio in both groups.
There was no significant difference in the mean heart rate of patients in the time interval before and after CO2 gas insufflation in both groups (p =0.169 and F (1, 58) =1.939) and also in the amount of changes of the mean heart rate in the two groups before and after CO2 gas insufflation (p =0.992 and F (1, 58) <0.001) Figure 3.
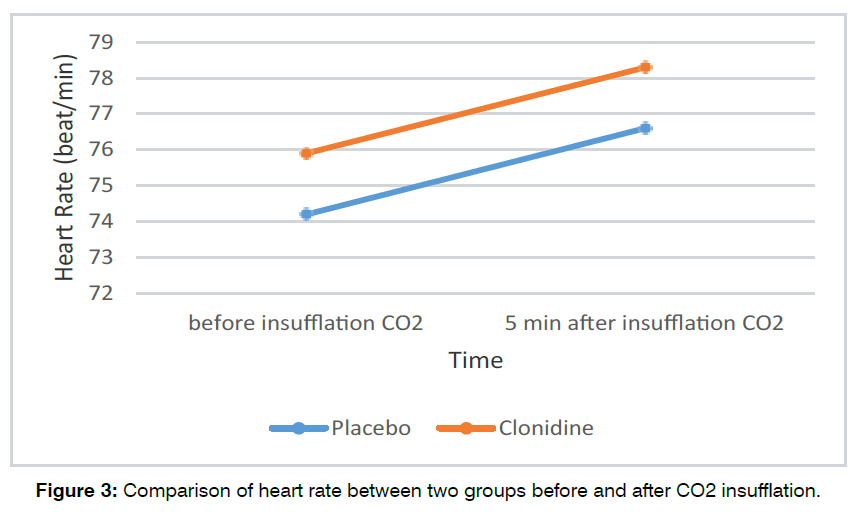
Figure 3: Comparison of heart rate between two groups before and after CO2 insufflation.
The mean arterial pressure in clonidine group was lower than the placebo group in all times except 15 and 30 minutes after CO2 insufflation, but this difference was statistically significant only at the time of instantly after intubation, before injection, and 5 minutes after insufflation of CO2 Table 3.
There was significant difference in the mean arterial pressure before and after laryngoscopy in both groups (F (1, 58) =31.85 and p <0.001) but the mean of these changes was not statistically significant in both groups (F (1, 58) =1.744 and p=0.192) and it increased with the same ratio in both groups.
The mean of arterial pressure in times before and after CO2 gas insufflation was statistically significant in both groups (F (1, 58) =16.28 and p <0.001) but the mean of these changes had no statistical difference in the two groups (F (1, 58) = 0.128 and p =0.722) and increased in both groups with the same ratio Figure 4.
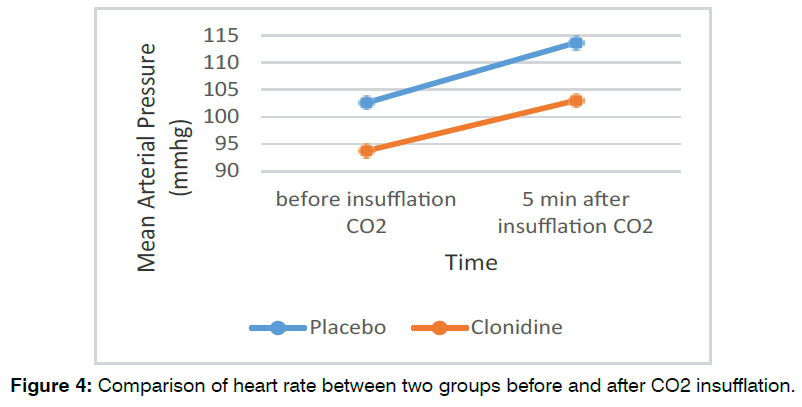
Figure 4: Comparison of heart rate between two groups before and after CO2 insufflation.
Time effect was significant on mean arterial pressure changes in both groups (intragroup p <0.001 and F (12, 696) =23.1) Figure 5.
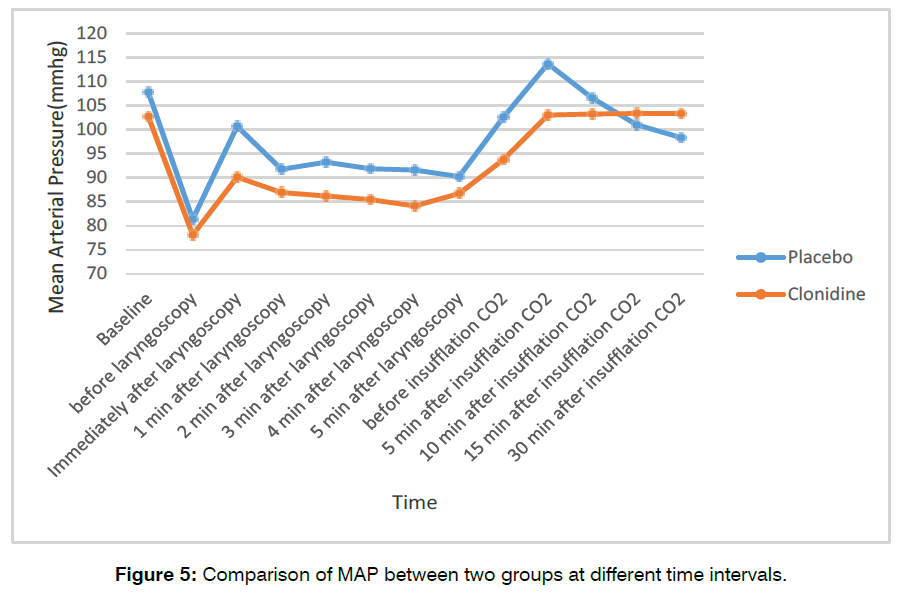
Figure 5: Comparison of MAP between two groups at different time intervals.
Five persons (16.7%) in each groups had postoperative shivering Table 4. This implies that both groups did not have any differences in postoperative shivering (p=1).
| Shivering score | Clonidine (N=30) | Placebo (N=30) | P-value |
|---|---|---|---|
| 0 | 25 (83.3) | 25 (83.3) | 0.572 |
| 1 | 3 (10) | 1 (3.3) | |
| 2 | 1 (3.3) | 1 (3.3) | |
| 3 | 1 (3.3) | 3 (10) | |
| 4 | 0 | 0 | |
| Total | 5 (16.7) | 5 (16.7) |
Table 4: Comparison of shivering score in study groups.
In terms of the need for atropine, ephedrine, and TNG, the following results were obtained: in clonidine group 1 patient received atropine and 1 patient received ephedrine and in placebo group 3 patients received atropine, 1 patient received ephedrine, and 1 patient received trinitroglycerin (TNG). Although the number of patients who needed medical intervention was lower in the clonidine group, Chi-2 square test result did not show any significant differences (p =0.228, and X2=1.456).
Discussion
Despite numerous advantages of laparoscopic cholecystectomy compared to surgery such as better maintenance of homeostasis or less postoperative pain [10], hemodynamic changes are a common problem during laparoscopy [11]. The aim of this study was to evaluate the effect of clonidine pretreatment on hemodynamic changes following endotracheal intubation and carbon dioxide insufflation and postoperative shivering in patients undergoing laparoscopic cholecystectomy.
Findings of our study on the effect of clonidine premedication on heart rate showed that the heart rate in the clonidine group was lower than the placebo group but the difference between the two groups was not statistically significant (P= 0.8). Also, findings showed that the mean blood pressure in the clonidine group was lower than the placebo group, but this difference was not statistically significant (P = 0.053).
These findings were consistent with the results of previous studies such as that showed the effect of clonidine as a premedication on hemodynamic changes during laparoscopic cholecystectomy12, the effects clonidine as a premedication on hemodynamic changes associated with laparoscopic cholecystectomy compared with ranitidine [13], the effect of clonidine premedication on the hemodynamic changes during laparoscopic cholecystectomy [14], the effect of oral clonidine premedication on the hemodynamic response of patients undergoing laparoscopic cholecystectomy [15], the effect of oral clonidine premedication on hemodynamic changes in patients undergoing laparoscopic cholecystectomy compared with the ranitidine [16] and the effect of premedication with oral clonidine on hemodynamic status during laparoscopic cholecystectomy [17]. All showed that in the clonidine group, the mean of increase in systolic and diastolic blood pressure after anesthesia and carbon dioxide insufflation was lower than the placebo group. Also, these studies have shown that the increase in heart rate after anesthesia was less in the clonidine group than in the placebo group. Contrary to the above findings, Colcarney et al. [18] study in 2016 on the effect of intravenous clonidine 1.5 μg / kg with lactate ringer as a premedication on the hemodynamic response of patients undergoing laparoscopic cholecystectomy compared with Ringer lactate alone, showed that the mean heart rate and blood pressure in the ringer lactate group were lower than the clonidine group.
It seems that clonidine surpasses the blood-brain barrier to target the central α2 adrenoreceptors to affect the central nervous system by reducing the brain’s sympathetic tone. This leads to a decrease in systolic and diastolic blood pressure and heart rate.
However, the agonist effects of the central alpha 2 adrenoreceptors are not the only route of action of clonidine, as it also has intrathecal effects when used as a supplementary drug in spinal or epidural anesthesia (with local anesthetics). Also, its peripheral effects are fully identified. These beneficial effects of clonidine have been demonstrated not only in adult patients but also in children and in patients under general anesthesia, axonal nerve block, and nerve block.
Recent studies suggest that the peripheral and neuroaxial effects of clonidine may have different mechanisms than what was previously identified as the role of clonidine as an alpha 2 adrenoreceptors agonist. Although this mechanism is unclear, some hypothetical mechanisms have been proposed, and a number of them have shown the role of clonidine in inhibiting tetrodotoxin-sensitive sodium channels. Further studies are underway in this field [19].
The CO2-induced pneumoperitoneum used for laparoscopic procedures is a complex pathophysiological phase with significant hemodynamic changes. Carbon dioxide is mainly used in this process because of it is colorless, non-combustible, highly soluble and permeable to tissues, which reduces the risk of gas embolism. Hemodynamic changes associated with pneumoperitoneum are the result of increased intraabdominal pressure and hypercarbia [20-22].
Five minutes after the onset of pneumoperitoneum, a significant increase in vasopressin and neurophysin occurs. Then, the concentration of vasopressin in plasma decreases; while the concentration of neurophysin reaches a steady state. Vasopressin level is consistent with Systemic Vascular Resistance (SVR) changes. Plasma concentrations of epinephrine, norepinephrine, and renin also increase during laparoscopy [23].
To reduce this hemodynamic response, a wide variety of factors are used in both premedication and induction. Researchers have used beta-blockers, alpha-2 agonists, magnesium sulfate, opioids, vasodilators, and gas-free approaches to counteract hemodynamic changes. Alpha 2 agonists were discussed until the early 1980s. The Euro Anesthesia Conference in 2003 extensively discussed the pharmacology of alpha 2 agonists and anesthesia [23].
Compared to other agents, the safety margin of clonidine for use in anesthesia is high. Clonidine acts as a presynaptic α2 receptor agonist in the nucleus Tractus Solitarii in the medulla [24-26]. The stimulation of these receptors suppresses the effects of sympathetic pathways, and therefore reduces the blood pressure and vascular tone in the heart, kidneys, and peripheral blood vessels.
In our study, intra-abdominal pressure was kept below 15 mm Hg. Studies have shown that intra-abdominal pressure greater than 15 mm Hg increases systemic vascular resistance, heart rate, vena cava pressure, and mean arterial pressure while decreasing stroke volume, and these effects are exacerbated in patients with elevated head position [21].
Our study showed no difference between the two groups receiving clonidine and placebo in terms of postoperative shivering. Contrary to our findings, Jabbari Moghadam et al. study [27] showed that shivering occurred in 10.7% of patients in the placebo group, while this rate was zero in the clonidine group.
Also, in the study of Nicola et al. [28], clonidine intake increased the threshold of individuals against coldinduced shivering. Their study showed that clonidine may inhibit the body’s thermoregulatory response to cold. The observed differences may be due to differences in the type of surgery, dose and timing of clonidine use, and differences in the study population of our research with the others.
Also, the findings of our study showed that the need for atropine, ephedrine, and TNG in patients in the clonidine group was less than the placebo group. In the clonidine group, 1 patient received atropine and 1 patient received ephedrine, while in the placebo group, 3 patients received atropine, 1 patient received ephedrine, and 1 patient received TNG. Consistent with our findings, in the study by Colcarney et al. [18], 23.33% of patients in Ringer lactate group and none of the patients in clonidine group required TNG.
In Bandari et al.’s study [13], none of the patients receiving clonidine needed nitroglycerin, while 28% of the patients in the ranitidine group needed nitroglycerin. In the Dos et al. study [16], the nitroglycerin was required in 33.3% of patients in the ranitidine group, while none of the patients in the clonidine group needed it. Also, other studies have shown that the administration of clonidine as a premedication in laparoscopic cholecystectomy is generally associated with maintaining hemodynamic stability and the absence of bradycardia or hypotension during surgery [14,28].
Limitations
The duration of follow-up of the patients is one limitation in this trial. And, another limitation of the present study was the effect of clonidine on postoperative pain which was not investigated.
Conclusion
This study showed that the oral administration of 150 micrograms of clonidine as a cheap and cost-effective premedication in patients undergoing laparoscopic cholecystectomy improves hemodynamic stability after intubation, and after insufflation of CO2.
Acknowledgement
The authors would like to offer their special thanks to the Research Deputy of Ardabil University of Medical Sciences for its support and providing funding for this research.
Author's Contribution
1. Study concept and design: ME & KhI 2. Acquisition of data: ME & MR 3. Analysis and interpretation of data: ME & KhI 4. Drafting of the manuscript: KhI & ME 5. Critical revision of the manuscript for important intellectual content: ME 6. Statistical analysis: KhI & MR 7. Administrative, technical, and material support: ME 8. Study supervision: ME
Conflicts of Interests
One of the authors is Anesthesiologist, but there are no conflicts of interest for declaration.
Ethical Statements
We obtained the approval of Ardabil University of Medical Sciences Ethics Committee and registered on the site www.irct.ir with registration number IRCT2016022716612N4 and obtained informed written consent from patients for participating in this research. This article does not contain personal information that allows to identify the patients.
References
- Kamali A, Ashrafi TH, Rakei S, Noori G, Norouzi A. A comparative study on the prophylactic effects of paracetamol and dexmedetomidine for controlling hemodynamics during surgery and postoperative pain in patients with laparoscopic cholecystectomy. Medicine. 2018;97(51).
- Hs P. N A. Effect of intravenous clonidine premedication on perioperative hemodynamic response in patients undergoing laparoscopic cholecystectomy: a case-control study. Int J Med Sci Public Health. 2016;5(6):1213.
- Feig BW, Berger DH, Dougherty TB, Dupuis JF, Hsi B, Hickey RC, et al. Pharmacologic intervention can reestablish baseline hemodynamic parameters during laparoscopy. Surgery. 1994;116(4):733-9.
- Ibrahim AN, Kamal MM, Lotfy A. Comparative study of clonidine versus esmolol on hemodynamic responses during laparoscopic cholecystectomy. Egypt J Anaesth. 2016;32(1):37-44.
- Bhandari D, Tidke S, Sharma V, Dongre H, Garg D, Dhande P. Hemodynamic changes associated with laparoscopic cholecystectomy: effect of oral clonidine premedication. IOSR J Pharm. 2012;2(4):72-7.
- Dar FA, Sadat S, Javed T, Lone AQ. Role of intravenous Clonidine hydrochloride in attenuating hemodynamic response to laryngoscopy, endotracheal intubation and pneumoperitoneum in patients undergoing elective laparoscopic cholecystectomy. Int J Biomed Adv Res. 2015;6(9):665-72.
- Singh S, Arora K. Effect of oral clonidine premedication on perioperative haemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2011;55(1):26.
- Shen H, Chen Y, Lu KZ, Chen J. Parecoxib for the prevention of shivering after general anesthesia. J Surg Res. 2015;197(1):139-44.
- Moghaddam MJ, Ommi D, Mirkheshti A, Dabbagh A, Memary E, Sadeghi A, et al. Effects of clonidine premedication upon postoperative shivering and recovery time in patients with and without opium addiction after elective leg fracture surgeries. Anesth Pain Med. 2013;2(3):107.
- Downs SH, Black NA, Devlin HB, Royston CM, Russell RC. Systematic review of the effectiveness and safety of laparoscopic cholecystectomy. Database of Abstracts of Reviews of Effects: Quality-assessed Reviews. 1996.
- Wahba RW, Béïque F, Kleiman SJ. Cardiopulmonary function and laparoscopic cholecystectomy. Can J Anaesth. 1995;42:51-63.
- Nayek SK, Sengupta M, Paul KK, Bhattacharjee DP, Paul S. Effects of clonidine on haemodynamics in patients undergoing laparoscopic cholecystectomy-a comparative study. Int J Pharm Chem Biol Sci. 2013;3(3).
- Bhandari D, Tidke S, Sharma V, Dongre H, Garg D, Dhande P. Hemodynamic changes associated with laparoscopic cholecystectomy: effect of oral clonidine premedication. IOSR J Pharm. 2012;2(4):72-7.
- Chandrashekaraiah MM, Upadya DM, Jayachandran SP, Wali M. Effects of clonidine premedication on hemodynamic changes during laparoscopic cholecystectomy-A randomized control study. Appl Cardiopulm Pathophysiol. 2011;15:91-8.
- Singh S, Arora K. Effect of oral clonidine premedication on perioperative haemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2011;55(1):26.
- Das M, Ray M, Mukherjee G. Haemodynamic changes during laparoscopic cholecystectomy: effect of clonidine premedication. Indian J Anaesth. 2007;51(3):205-10.
- MR R. Evaluation of oral clonidine premedication on hemodynamic parameters during laparoscopic cholecystectomy.
- Kulkarni K. Effect of Intravenous Clonidine as Premedication on Haemodynamic Responses during Laparoscopic Cholecystectomy. J Anesth Crit Care Open Access. 2016;4(1):00121.
- Safran DB, Orlando III R. Physiologic effects of pneumoperitoneum. Am J Surg. 1994;167(2):281-6.
- Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110(3):810-5.
- Liu SY, Leighton T, Davis I, Klein S, Lippmann M, Bongard F. Prospective analysis of cardiopulmonary responses to laparoscopic cholecystectomy. J Laparoendosc Adv Surg. 1991;1(5):241-6.
- Baratz RA, Karis JH. Blood gas studies during labaroscopy under general anesthesia. Anesthesiology. 1969;30(4):463-4.
- Maze M. Pharmacology and Use of Alpha-2 agonists in Anesthesia. Eur J Anaesthesiol. 2003:37-43.
- Keränen A, Nykänen S, Taskinen J. Pharmacokinetics and side-effects of clonidine. Eur J Clin Pharmacol. 1978;13:97-101.
- Baillie TA, Davies DL, Davies DS, Hughes H, Neill E. The metabolism of clonidine and related imidazoline derivatives in rat liver. Br J Pharmacol. 1978;63(2):400P.
- Moghaddam MJ, Ommi D, Mirkheshti A, Dabbagh A, Memary E, Sadeghi A, et al. Effects of clonidine premedication upon postoperative shivering and recovery time in patients with and without opium addiction after elective leg fracture surgeries. Anesth Pain Med. 2013;2(3):107.
- Nicolaou G, Chen AA, Johnston CE, Kenny GP, Bristow GK, Giesbrecht GG. Clonidine decreases vasoconstriction and shivering thresholds, without affecting the sweating threshold. Can J Anaesth. 1997;44:636-42.
- Sung CS, Lin SH, Chan KH, Chang WK, Chow LH, Lee TY. Effect of oral clonidine premedication on perioperative hemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Sin. 2000;38:23-30.
1Department of Anesthesiology, School of Medicine, Ardabil University of Medical Sciences, Ardebil, Iran
2Department of Anesthesiology, School of Medicine, Ardabil University of Medical Sciences, Ardebil, Iran
3School of Medicine, Ardabil University of Medical Sciences, Ardebil, Iran
Send correspondence to:
Khatereh Isazadehfar
Determinants of Health Research Center, Department of Community Medicine, School of Medicine, Ardabil University of Medical Sciences, Ardabil, Iran E-mail: isazadehfar@yahoo.com
Paper submitted on October 27, 2023; and Accepted on November 16, 2023
Citation: Isazadehfar K. The Effect of Clonidine Premedication on Hemodynamic Changes Following Tracheal Intubation and CO2 Gas Insufflation and Postoperative Shivering In Patients Undergoing Laparoscopic Cholecystectomy; a Randomized Clinical Trial. Int Tinnitus J. 2023;27(2):174-182.


