The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 26, Issue 1 / June 2022
Original Paper Pages:1-10
10.5935/0946-5448.20220001
The Effectiveness of Mindfulness-Based Cognitive Therapy in the Management of Tinnitus
Authors: Chanchai Jariengprasert, Kasinee Watanapornmongkol, Sivaporn Kiatthanabumrung, Tosapohn Wisupagan
PDF
Abstract
Mindfulness-based cognitive therapy (MBCT) has been suggested as an effective modality in reducing the effects of tinnitus and improving quality of life. This article aimed to compare the effectiveness of MBCT with that of standard treatment in the management of tinnitus in Thai patients. All participants were voluntarily divided into experimental MBCT and control groups depending on their availability. In addition to educational sessions and standard treatment, the MBCT group completed four weekly 120-minute sessions of mindfulness practicing skills. The Thai version of the Tinnitus Handicap Inventory (THI-T) and Hospital Anxiety and Depression Scale (HADs-T) were administered at baseline, 4th week, and 12th week. Tinnitus intensity (dB) was measured at baseline and 12th week. All data were compared between the different time points, within each group, and between the two groups. A total of 45 patients were enrolled, 24 in the MBCT group and 21 in the control group. When comparing baseline to post-treatment measurements, statistically significant improvements were observed in all outcomes except tinnitus intensity in both groups. The THI-T and HADs-T scores in the MBCT group were significantly lower than those in the control group at the 12th week. The reduction in the THI-T scores, HADs-T scores, and tinnitus intensity tended to be greater in the MBCT group after the 4-week course and at the 3-month follow-up assessment. The MBCT showed benefits in the management of tinnitus in terms of improved THI-T and HADs-T scores, and overall quality of life
Keywords: Tinnitus, Mindfulness therapy, Cognitive behavioral therapy.
Introduction
Tinnitus is a sound disturbance, perceived in one or both ears, that occurs without an external source. This sound can have many characteristics, such as ringing, clicking, buzzing, and fuzz, and in some cases, has been described as similar to the sound of crickets. In the United States, more than 50 million patients [1] are affected, and tinnitus has a global prevalence of ”10%–30% [2,3,4].” Of those with tinnitus, 10%–15% experience severe symptoms that impact quality of life, such as insomnia, irritability, or anxiety [3,4,5]. In addition, about 2%–5% of people with tinnitus encounter mental health problems such as depression, anxiety, and cognitive dysfunction. There have been reports of patients feeling suicidal idea because of tinnitus-related symptoms [6].
Many factors can stimulate the symptoms of tinnitus, and it can occur in people with normal hearing and those who are hearing impaired. However, individuals with hearing impairments are twice as likely to develop tinnitus. Tinnitus has often been reported to be associated with aging. However, despite the age-dependent occurrence of hearing impairment, no relationship has been found between age and tinnitus incidence [7].
There are two main types of tinnitus: subjective and objective tinnitus. Subjective tinnitus is often caused by hearing disorders or abnormalities in the auditory pathway, which can occur in the outer, middle, or inner ear, the auditory nerve, or the central nervous system. In contrast, objective tinnitus is caused by a real sound, i.e., that produced by a vascular structure near the ear. Such sounds can be produced by abnormalities in blood vessels, such as arteries that are abnormally connected with veins (A-V fistula, malformation), an aneurysm, or abnormal muscle twitching in the middle ear. Although there is no definite pathogenesis for idiopathic subjective tinnitus, one theory proposes that the symptoms are related to a neurotransmitter disorder elicited by injury in the peripheral auditory nervous system [7]. In a validated model of tinnitus and hyperacusis [8], biochemical studies provided evidence that cochlear damage induced longterm alterations to inhibitory synapses at various levels of the auditory system, leading to central gain enhancement. Multiple neuronal mechanisms with distinct temporal and spectral profiles could mechanistically contribute to central gain enhancement, including: 1) a decrease in inhibitory synaptic responses; 2) an increase in excitatory synaptic responses; or 3) alterations to intrinsic neuronal excitability.
The characteristics of tinnitus symptoms depend on the perception and responses of the individual. Many tools have been developed to assess the causes, severity, and impact of tinnitus on patients, with the goal of helping physicians develop a management plan. Tinnitus assessments can be divided into 2 categories [1]. The first involves audiometric evaluations of hearing loss, such as audiograms, tympanograms, acoustic reflex testing, and otoacoustic emission testing, and evaluations of tinnitus symptoms, such as pitch and intensity matching, tinnitus masking, and residual inhibition. The second involves assessments of severity and the impact of tinnitus in terms of activities of daily living, including mental health and daily cognition. Clinically, it is believed that the level of the sound heard by the patient (i.e., loud or soft) may not be as important as how it affects the patient’s quality of life.
Currently, the tools available for measuring the severity and impact of tinnitus include the Tinnitus Handicap Inventory (THI), Tinnitus Reaction Questionnaire (TRQ), Tinnitus Functional Index (TFI), Tinnitus Severity Index (TSI), and Visual Analog Scales (VAS). The THI, invented in 1996, was designed to assess the impact and effectiveness of tinnitus treatment [9]. It consists of 25 items with 3 areas: a functional subscale (12 items), emotional subscale (8 items), and catastrophic response subscale (5 items). For each item, there are three response options: “Yes “(4 points,” Sometimes (2 points) and “No” (0 points). The total score ranges from 0–100 points, and can be grouped to reflect 5 levels of handicap: 0–16 for no handicap (Grade I), 18–36 for mild handicap (Grade II), 38–56 for moderate handicap (Grade III), 58–76 for severe handicap (Grade IV), and 78–100 for catastrophic handicap (Grade V). In 2012, the Thai version of the THI (THI-T) was translated, and it was found to have good internal consistency and reliability for the total, functional, emotional, and catastrophic scales (a=0.902, 0.804, 0.831 and 0.661, respectively). Further, scores on the THI-T were found to significantly correlate with those on the 36-item short-form health survey and a visual analog scale, indicating that it could be used to reliably assess the severity of tinnitus, including evaluations of treatment [10].
Tinnitus treatment is based on the cause and physiological features of the condition in each individual. Chronic tinnitus is difficult to treat, as most patients do not respond to treatments. For idiopathic subjective tinnitus, there are a variety of treatment methods, including counseling and reassurance, the use of a tinnitus masker, and hearing aids in hearing-impaired patients. Medication, acupuncture, transcutaneous electrical nerve stimulation, and cognitive behavioral therapy have all been examined for the treatment of tinnitus [1,11,12]. Although some guidelines have been suggested, there are no standard treatments that have been found to effectively cure or improve symptoms in all patients [13]. As a result; the main goal of treatment is to reduce tinnitus loudness, associated stress, and the impact on mental health, thus enabling patients to lead a normal life.
Studies have shown that psychosocial factors and cognitive processes have a profound effect on human physical health [14,15,16]. In 2004, Londero et al. proposed a theory regarding the relationship between the central auditory pathway and the limbic system, which deals with perception, emotional awareness, behavior, and cognition [17]. This theory may be useful in explaining the cause of tinnitus, and thus support the application of treatments based on cognitive and behavioral therapy, which have been recommended in some cases [17-20].
Mindfulness-based cognitive therapy (MBCT): Since an introduction of the concept of mindfulness, the new mode of healing, many studies have been reported exponentially in the world of medicine. The effectiveness of MB stress reduction program (MBSRP) in the treatment of anxiety disorders had been demonstrated [21]. Mindfulness involves attending to relevant aspects of experience in a nonjudgmental manner. In this challenging technique, an individual focuses their awareness of the emotions and thoughts that occur at each moment, and works to change how their mind responds to stimuli. Instead of permitting habituated responses to dominate cognition, MBCT encourages individuals to recognize and respond to stimuli consciously. The goal is to commit to what is happening right now by maintaining awareness on each moment as it happens, and to resist using emotions to determine what is happening in a situation. To this end, practitioners aim to disengage from strong attachments to beliefs, thoughts, and emotions, thereby developing a greater sense of emotional balance and well-being. Mindfulness might influence susceptibility to, or enhance the ability to recover from, disability and disease in a number of ways, including 1) decreased perception of pain severity; 2) increased ability to tolerate pain or disability; 3) reduced stress, anxiety, or depression; 4) diminished usage of analgesic, anxiolytic, or antidepressant medication; 5) enhanced ability to reflect on choices regarding medical treatments; 6) improved adherence to medical treatments; 7) increased motivation regarding lifestyle changes; 8) enriched interpersonal relationships and social connectedness; and 9) alterations in biological pathways affecting health [22].
Many studies have suggested that MBCT can cause physiological changes in stress or chronic depression. It has also been found to decrease the secretion of cortisol in the body, and to influence anatomical structures in the brain [23]. Davidson et al. found that individuals who engaged in MBCT exhibited a significant increase in leftsided anterior activation, which is associated with positive affect, and a significant increase in antibody titers after an influenza vaccine compared with those in a control group. The magnitude of the increase in left-sided activation predicted the magnitude of the increase in antibody titers after receiving the vaccine. Even a short course of MBCT produced demonstrable positive changes in both brain activity and immune function [24]. Sadlier et al. reported that MBCT led to significantly reduced scores on both the Hallem tinnitus questionnaire and the tinnitus VAS [25]. Using the resting state functional connectivity MRI (rsfcMRI) data, Roland et al. reported increased connectivity in attention networks but not in the default mode network following an eight-week MBSRP. The mindfulness group also exhibited a decrease in symptoms of tinnitus and depression. They concluded that, as it is both noninvasive and inexpensive, MBCT is a promising treatment option for chronic tinnitus [26].
Several randomized controlled trials (RCTs) have compared the effectiveness of mindfulness meditation to that of relaxation therapy for treating tinnitus [27-29]. Phillippot et al. reported that the effects of psychoeducation were maintained in the MBCT group, while they declined in the relaxation group. Neither the MBCT nor relaxation training led to immediate improvement; this was likely because of the large effect already elicited by the psychoeducation intervention. However, the use of cognitive control as an unhealthy coping method tended to decrease in the MBCT group. It is possible that the benefits of mindfulness would have been stronger if the intervention had been conducted for a longer period of time [27].
Kreuzer et al. conduced a RCT to study the efficacy of a specific mindfulness- and body-psychotherapybased program in 36 patients with chronic tinnitus. The primary outcome, the change in tinnitus complaints, was measured using the German version of the Tinnitus Questionnaire (TQ). The results showed a significant improvement in TQ scores from the baseline to week 9 in both groups, but the degree of improvement was greater in the mindfulness group [28].
Arif et al. conducted a RCT in 86 patients. Of the original group, 34 completed a mindfulness meditation program and 27 completed a relaxation therapy program. Both the mindfulness meditation and the relaxation therapy programs led to significant improvements in all outcome measures, except one. However, the mindfulness group exhibited a significantly greater reduction in TRQ score. This suggests that both treatments were effective in the management of tinnitus, although mindfulness meditation was superior to relaxation therapy [29].
Another RCT comparing MBCT (n=39) to relaxation therapy (n=36) indicated that both interventions led to significant reductions in tinnitus severity and loudness, as well as associated psychological distress, anxiety, depression, and disability. MBCT led to a significantly greater reduction in tinnitus severity compared with relaxation therapy, and the effects persisted for 6 months. The researchers concluded that, compared with intensive relaxation therapy, MBCT was more effective in reducing tinnitus severity, psychological distress, and disability in chronic tinnitus patients, regardless of initial tinnitus severity, duration, or hearing loss [30].
In Thailand, MBCT has been used to treat depression and anxiety. In 2012, Areekit et al. conducted a semi-experimental study with 20 patients each in an experimental and control group. They found that the Beck Depression Inventory Scale scores were significantly lower in the MBCT versus the control group, indicating that the method was effective for treating depression [31].
However, the effectiveness of MBCT for treating tinnitus has not been studied in Thailand. To address this, we conducted a pilot study to establish the feasibility and effectiveness of MBCT in Thai tinnitus patients. We evaluated the THI-T score, Thai version of the Hospital Anxiety and Depression Scale score (HADs-T), and tinnitus intensity (dB) before and after treatment, and compared these with values obtained from a control group. We hypothesized that MBCT would lessen the effects of tinnitus and improve the quality of life in the tinnitus patient group.
Methods
This study had a quasi-experimental design. We examined the effectiveness of MBCT in patients with tinnitus according to data collected before and after an intervention in two patient groups. The study was approved by the Human Ethics Committee, ID11-60-58, from the Faculty of Medicine, Ramathobodi hospital.
Participants: Participants were patients with tinnitus who sought treatment at the Outpatient ENT clinic at the Faculty of Medicine, Ramathibodi Hospital, Mahidol University during the period from February to November 2018. The inclusion criteria were: age of 18 years or older, and course of tinnitus lasting at least 3 months. We excluded patients with middle ear problems such as eardrum perforation, infection, or effusion, as well as those with neurological conditions, brain diseases, and major psychiatric disorders.
The research process was described to all patients, who were then asked to sign an informed consent form and complete a personal information form if they wanted to participate in the study. All volunteers were given detailed descriptions of the treatment program and asked to join either the control or MBCT group depending on their availability. If participants declined MBCT or were not available to attend all of the program sessions, they were assigned to the control group.
Instruments and tools
The THI-T consists of 25 items encompassing the Functional subscale (12 items), Emotional subscale (8 items), and Catastrophic response subscale (5 items). (10)
The HADs-T consists of 14 questions (anxiety and depression subscales, 7 items each, for a total of 21 points). If a subscale score was greater than or equal to 11, this was considered to indicate abnormal levels of anxiety or depression [32].
The THI-T and HADs-T were administered in all participants three times: before treatment, after 4 weeks, and after 12 weeks of treatment.
A trained audiologist used a GSI-61 audiometer (Grason Stadler Inc., Eden Prairie, Minnesota, USA) to conduct tinnitus evaluations. They used the principle of tinnitus sound matching, including matching of pitch (Hz) and loudness (dB). The loudness level that matched the tinnitus intensity was evaluated in all participants twice: once before treatment and once 12 weeks afterwards
Procedures
All participants completed the THI-T and HADs-T questionnaires and underwent a tinnitus evaluation prior to treatment. Standard treatment for tinnitus was provided to both groups, including counseling to educate patients about the condition, causes, symptoms, treatment methods, and prognosis. They were given advice and strategies, including self-masking, wearing hearing aids for hearing-impaired individuals, and follow-up monitoring. The participants in the control group were asked to visit the center to undergo evaluations before the intervention began and at 4 and 12 weeks afterwards.
Experimental group: The MBCT activities took place during one 120-minute session per week for 4 consecutive weeks, led by a team including a psychiatrist, otolaryngologists, and an audiologist. Each session was led by one member of the team, and the activities in each session were as follows.
Session 1: The participants learned how to practice mindfulness according to the MBCT theory. A game or role-playing scenario was used to teach the basic sensations associated with mindfulness. The participants were asked to adhere to this principle for at least 15 to 30 minutes every day during the first week.
Session 2: The participants received basic information about the disorder, causes, symptoms, methods of treatment, and prognosis to help them accept and understand their condition. They were asked about the practical results of their MBCT practice, and encouraged to apply this principle more frequently, such as during three 30-minute sessions per day. They were also given the opportunity to ask questions and exchange experiences with the other group members.
Session 3: The facilitator introduced the concept of selfmasking and associated methods. They provided basic information about the assessment of tinnitus, hearing impairments, and treatment options such as tinnitus masking using a hearing aid, masker, hearing aid with a masker, and self-masking using natural sound sources. Several free mobile phone applications were recommended for tinnitus management. The participants were followedup again regarding the practical results of their MBCT practice, and were encouraged to apply this principle more frequently, such as during a 5–10 minutes session every hour. The group completed a question and answer period.
Session 4: The lessons were reviewed and the guidelines for MBCT were summarized with a focus on the continued use of this principle in daily life. All participants were given the opportunity to exchange their experiences with the other group members.
Statistical analysis: The data were analyzed using PASW statistics 18.0. A p value < 0.05 was considered statistically significant. Descriptive statistics included the mean, standard deviation, (SD), median (P25th–P75th), and percentage (%). The data distribution was tested using the Shapiro–Wilk test. Independent t-tests and the Mann–Whitney test were used to compare differences between groups for continuous data with a normal distribution. The Chi-squared test was used to compare data collected before the intervention, at 4 weeks, and 12 weeks afterwards within groups. A repeated measure ANOVA with multiple comparisons via the Bonferroni method was used to compare results between the two groups.
Results
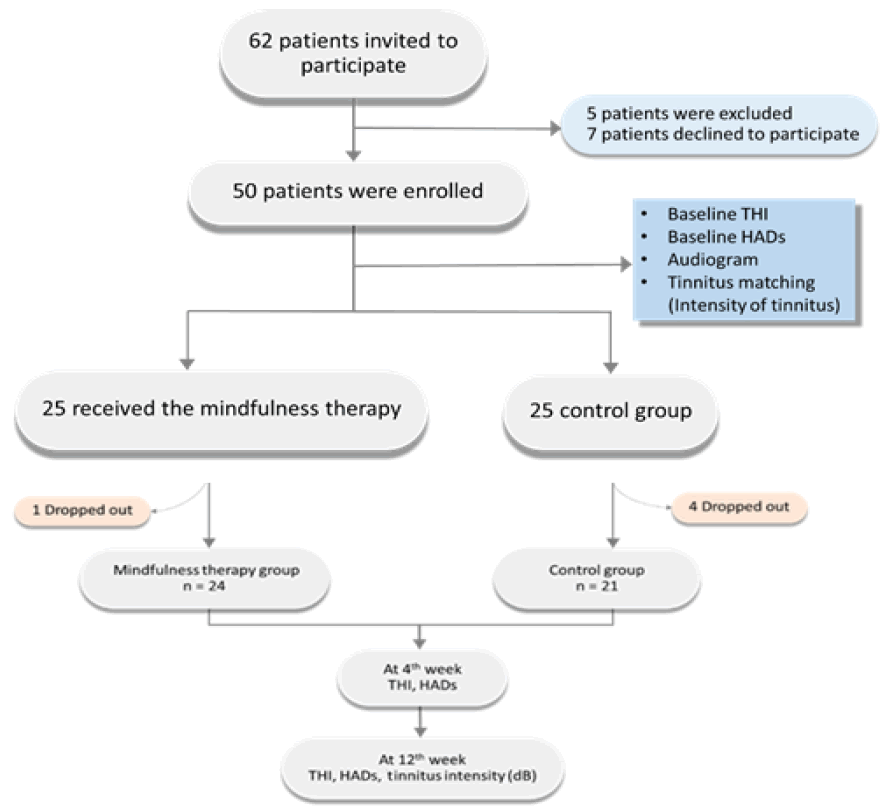
Sixty-two patients were initially invited to participate in this study. Of these, 5 were excluded because of middle ear problems or neuro-psychiatric conditions, and 7 declined to participate. Table 1 shows the baseline characteristics of the participant group. There were 50 participants, 19 men (38%) and 31 women (62%), ranging in age from 25 to 79 years. The participants were divided evenly into an MBCT and a control group. There was no difference in baseline characteristics between the groups. During the treatment period, 4 patients from the control group and 1 from the MBCT group dropped out of the study because of scheduling limitations.
| Total (n = 50) |
MBCT group (n = 25) | Control group (n = 25) |
p-Value | |
|---|---|---|---|---|
| Age (years) | 60.02 ± 14.04 | 61.48 ± 12.48 | 58.56 ± 15.56 | 0.468 |
| Gender (M/F) | 19/31 | 10/15 | 9/16 | 0.771 |
| Duration of symptoms (weeks) | 72 (24–148) | 52 (24–158) | 96 (24–146) | 0.884 |
| Baseline THI-T score | 28.1 ± 15.51 | 27.48 ± 14.93 | 28.72 ± 16.36 | 0.781 |
| Baseline HADs-T score (Anxiety subscale) (Depression subscale) |
5 (2–7) 3 (2–6) |
5 (2–7.5) 3 (1–4) |
5 (2–7) 4 (2–6.5) |
0.915 0.074 |
| Baseline hearing – PTA (dB) | 39.08 ± 20.58 | 35.12 ± 19.47 | 43.04 ± 21.28 | 0.176 |
| Baseline tinnitus intensity (dB) median (range) |
42 (22.25–51.50) |
42 (11.0–53.75) |
35 (22.25–51.50) |
0.938 |
| Lateralization (unilateral/bilateral), n (%) | 37/17 (68.5/31.5) | 15/10 (60/40) | 28/7 (72/28) | 0.370 |
| Hearing aid, n (%) | 5 (10) | 2 (8) | 3 (12) | 1.000 |
| Drugs, n (%) | 25 (50) | 13 (52) | 12 (48) | 0.777 |
| Acupuncture, n (%) | 3 (6) | 2 (8) | 1 (4) | 1.000 |
MBCT: Mindfulness-based cognitive therapy; M: male; F: female; THI-T: Thai version of the Tinnitus Handicap Inventory, HADs-T: Thai version of the Hospital Anxiety and Depression Scale, PTA: pure tone average
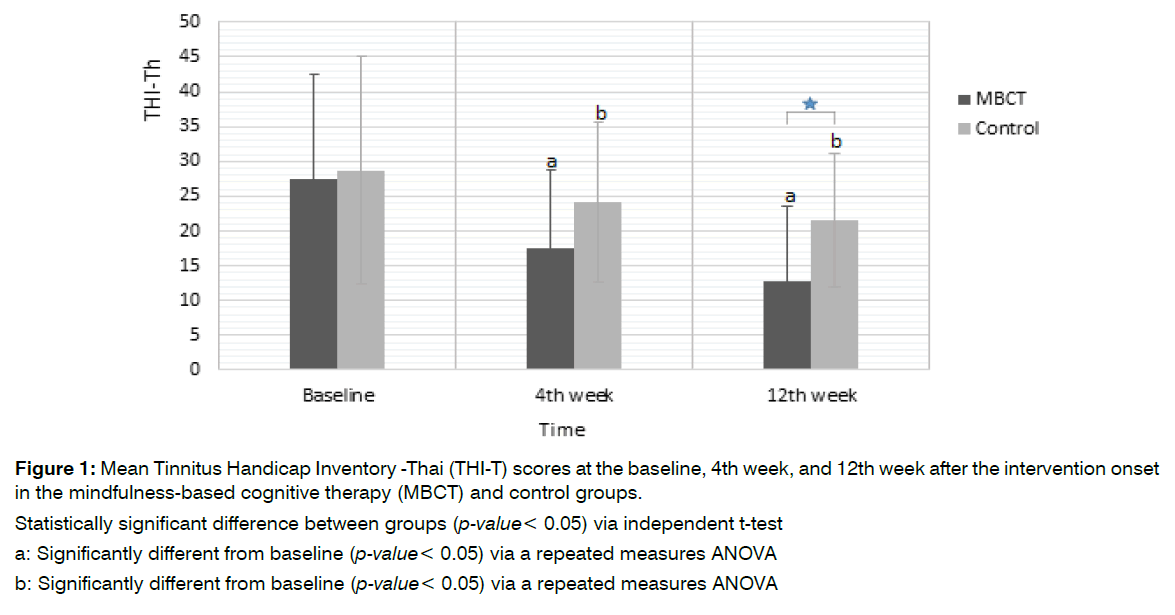
THI-T: Figure 1 shows the THI-T scores at the baseline, at 4 weeks, and at 12 weeks after the intervention onset in both groups. The mean THI-T scores in both groups decreased significantly at the 4- and 12-week assessments. However, at the 12th week, the mean THI-T score in the MBCT group was significantly lower than that in the control group (12.75 ± 10.78 vs. 21.62 ± 9.60; 95%CI −15.04, −2.69, p=0.006). We also found that the mean pre–post difference in THI-T score reduction tended to be greater in the MBCT group than in the control group at the 4th week (10.13 ± 14.26 vs. 6.57 ± 9.38) and at the 12th week (14.88 ± 16.24 vs. 9.14 ± 11.74).
Figure 1: Mean Tinnitus Handicap Inventory -Thai (THI-T) scores at the baseline, 4th week, and 12th week after the intervention onset in the mindfulness-based cognitive therapy (MBCT) and control groups.
Statistically significant difference between groups (p-value< 0.05) via independent t-test
a: Significantly different from baseline (p-value< 0.05) via a repeated measures ANOVA
b: Significantly different from baseline (p-value< 0.05) via a repeated measures ANOVA
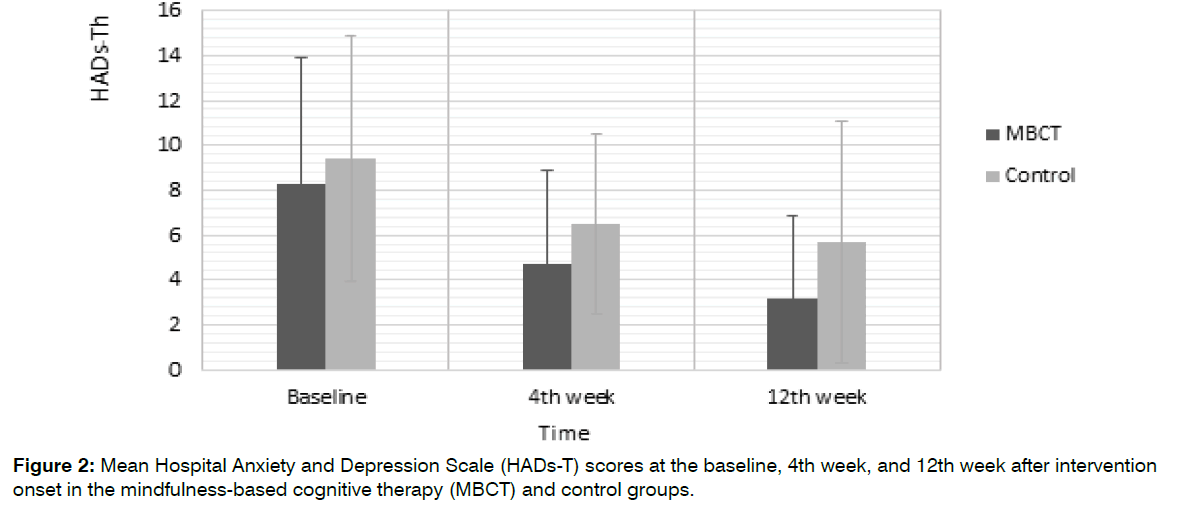
HADs-T: Figure 2 shows the average HADs-T scores at the baseline, at 4 weeks, and at 12 weeks after treatment onset. Participants in both groups had significantly lower HADs-T scores after the intervention. Although the MBCT group tended to have a greater reduction in HADs-T score compared with the control group, this was not significant at the 4th (3.71 ± 3.93 vs. 3.38 ± 3.41) or 12th (5.29 ± 4.23 vs. 4.24 ± 4.55) week after treatment onset.
Figure 2: Mean Hospital Anxiety and Depression Scale (HADs-T) scores at the baseline, 4th week, and 12th week after intervention onset in the mindfulness-based cognitive therapy (MBCT) and control groups.
Tinnitus intensity: The mean tinnitus intensity (dB) at the baseline was not significantly different from that at the 12th week in either the MBCT group (36.00 ± 22.64 vs. 26.25 ± 22.59) or control group (36.25 ± 22.07 vs. 31.38 ± 29.87). Further, we found no significant differences between the groups. However, the MBCT group had a tendency to exhibit more improvement (intensity reduction) compared with the control group (9.75 ± 20.27 vs. 4.88 ± 12.14) at 12 weeks after the treatment (Table 2).
| Tinnitus intensity mean ± SD (dB) | |||||
|---|---|---|---|---|---|
| Outcome | MBCT (n = 24) |
Control (n = 21) |
Mean difference (n = 45) | 95% CI difference | p-value |
| Baseline | 36.00 ± 22.64 | 36.25 ± 22.07 | −0.25 | −21.75, 21.25 | 0.981 |
| 12 weeks | 26.25 ± 22.59 | 31.38 ± 29.87 | −5.13 | −29.74, 19.49 | 0.667 |
| Week 12 vs. baseline | 9.75 ± 20.27 | 4.88 ± 12.14 | 4.88 | −11.96, 21.71 | 0.551 |
Table 2: The mean tinnitus intensity at the baseline and 12th week after treatment in the mindfulness-based cognitive therapy (MBCT) and control groups, and the improvement (intensity reduction) between both groups.
Flow chart showing patient participation at the beginning of the study and the drop-out rate during the intervention.
Discussion
In this study, we compared a MBCT intervention to a standard course of treatment in patients with tinnitus. Although both groups exhibited lower THI-T scores at the 4th and 12th weeks after the intervention onset, the participants in the MBCT group demonstrated a greater degree of improvement than those in the control group. These findings are consistent with previous reviews [27-30] and recent reports [33-35]. Using the Cochrane Database of Systematic Reviews, Fuller et al. selected 28 studies with a total of 2733 participants who had had tinnitus for 3 months or more. The participants ranged in age from 43 to 70 years, and underwent cognitive behavioral therapy (CBT) programs that lasted from 3 to 22 weeks in hospitals or online. The researchers concluded that CBT appeared to be effective in reducing the negative impact of tinnitus on quality of life in patients with rare adverse effects [36].
In the MBCT group in the present study, the average reduction in THI-T score at the 4th week, relative to the baseline, was 10.13 ± 14.26 points, and that at the 12th week was 14.88 ± 16.24 points. These values are above the minimal clinically important difference level for the THI (a reduction of 7 points). In contrast, in the control group, the average reduction in THI-T score at the 4th week was 6.57 ± 9.38, and that at the 12th week was 9.14 ± 11.74. Thus, the efficacy of the MBCT program appeared to increase over time, which is consistent with previous research [27-35]. Unfortunately, we did not collect data at 6 or 12 months in our study.
In a previous study, a standardized 8-week MBCT program administered to 182 adults with chronic distressing tinnitus (the largest sample group to date) led to significant and reliable improvements in tinnitusrelated distress and psychological distress in 50% and 41.2% of all patients, respectively, at a 6-week followup assessment. Increases in mindfulness and tinnitus acceptance explained unique post-intervention changes in tinnitus-related and psychological distress [33].
A systematic review of seven articles (425 patients), including three RCTs, three cohort studies, and one comparative controlled trial, evaluated the effects of different types of mindfulness-based interventions (MBIs), including MBCT and MBSR, according to the results of various questionnaires. Two of the three RCTs and six of the seven studies reported a statistically significant decrease in tinnitus distress scores directly after treatment in the MBI group. Further, one of the three RCTs reported a statistically significant improvement in depression questionnaire scores directly after MBI treatment, compared to a control group. Given the moderate to high quality of the studies, the investigators concluded that MBIs led to a post-therapy decrease in tinnitus distress scores, despite the heterogeneity of the patients, study design, type of MBI, and outcome assessments. No effects of MBIs were observed for depression and anxiety in tinnitus patients. The investigators suggested that mindfulness may have a role in tinnitus therapy; however, the long-term effects remain uncertain [34].
In the present study, although HADs-T scores tended to decrease in the MBCT group, no significant differences were found between groups. This is consistent with many previous studies [18,25] and also the review by Fuller36, who reported that although HADs scores tended to decrease after MBCT, these differences were not statistically significant, even in a study that administered cognitive behavioral therapy (CBT) for 12 months. Indeed, they reported that the benefit of CBT in terms of reducing symptoms of depression was minimal, and that evidence for CBT-induced improvements in anxiety, health-related quality of life, and negatively biased interpretations of tinnitus was limited. However, they did not separate MBCT from other types of cognitive therapy [36].
In terms of tinnitus management, the control group in the present study showed improvement after the standard intervention, received without attending the MBCT sessions. Therefore, MBCT appears to be a suitable additional treatment for patients with tinnitus, as it is likely to help improve their quality of life. However, the MBCT did not significantly reduce anxiety or stress, even though it has been reported to significantly benefit patients with anxiety and depression.
It is likely that a longer duration of regular MBCT practice is needed before patients adapt their new skills to daily activities. According to a set of guidelines for the treatment of tinnitus, there is no cure for this condition, and so whenever the noise is present, patients are likely to experience anxiety [37].
In terms of the effect of MBCT in reducing tinnitus intensity, we found no statistically significant differences before versus after the treatment in either group. However, the MBCT group tended to exhibit a greater pre–post intervention difference compared to the control group. These findings correspond to those of Kreuzer et al28, who reported that MBCT did not reduce the level of tinnitus. Tinnitus loudness can be evaluated in many different ways, and many studies have used questionnaires for this purpose [28,33,34,36]. In this study, we measured tinnitus loudness using auditory matching to identify the precise intensity in dB. We found that after the intervention the loudness decreased by 9.75 ± 20.27 dB in the MBCT group and 4.88 ± 12.14 dB in the control group. However, no statistical significance could be demonstrated.
A recent pilot study used voxel-based morphometric analysis of structural magnetic resonance imaging (MRI) scans to reveal clusters in the bilateral superior frontal gyrus that exhibited significant increases in gray matter volume throughout a mindfulness intervention and follow-up period. Further, gray matter changes in the occipital and cingulate regions were correlated with declines in tinnitus-related disability. Accordingly, the authors supported MBCT as an adequate approach for treating distressing symptoms of tinnitus, and suggested that neuroanatomical changes may reflect reductions in tinnitus-related severity [35]. In efforts to reduce the volume of tinnitus sounds in a specific case of tinnitus, a combination of treatments, such as hearing aids, a tinnitus sound masker, and mindfulness practice could produce an optimal outcome.
Tinnitus is a biopsychosocial condition, and the distress associated with the symptoms is affected by cognitive, behavioral, attentional, and social factors. This makes it a life-altering condition that can affect the thoughts, emotions, attention, behavior, and social world of a patient. In a healthcare journey study titled ‘Living with Tinnitus’, chronic distress was intensified by unhelpful health communications and alleviated by early interventions that offered clear, helpful, and realistic information about tinnitus and appropriate treatments [37].
Although it has overlap with other forms of CBT, MBCT is a unique approach to treating tinnitus. The key processes of sustained and flexible attention are targeted, and avoidance is reduced by increasing intentional exposure to the sensory experience of tinnitus. The cognitive behavioral element of the practice teaches individuals to recognize irritating stimuli (self-awareness) and consciously respond to them (self-acceptance and nonjudgment) or relearn to cope with them (patience, let-go, friendliness, self-compassion, etc.), with the goal of reducing the impact of tinnitus on daily life38. As reported by Marks et al., MBCT helps people to develop a long-lasting, radically different, and more helpful relationship with their tinnitus symptoms by shifting their attitude from being “at war” with tinnitus to “allowing it to be”. This process includes the development of mindful awareness, the experience of being in a group, embodied teaching, compassion, gratitude, and having an open mind.
Thus, MBCT can be successfully applied to tinnitus patients in a way that changes the factors that maintain tinnitus-related distress. This has led to its inclusion in many guidelines regarding tinnitus treatment [39,40].
As reviewed by Ludwig and Kabat-Zinn, mindfulness, historically a Buddhist practice (so-called “Sati” in Pali), can be considered as the universal human capacity to foster clear thinking and openheartedness. As such, this form of meditation requires no particular religious or cultural belief system. The original purpose of mindfulness in Buddhism—to alleviate suffering and cultivate compassion—suggests a potential role for this practice in the activities of medical patients and practitioners [22].
In Thai culture, Buddhism is the most commonly practiced religion. Buddhism involves learning the moral precept, the Middle Way practice, the Eightfold Path, and to ease the mind using various styles of meditation. These include “Samatha” and “Vipassana”, which can both be used to cultivate mindfulness [41]. Generally, for chronic non-life threatening conditions such as subjective tinnitus, Thai physicians, along with other physicians around the world, usually tell their patients that their condition is not harmful and that with time it may cease or they will get used to it. It is possible that compared with patients in other countries, Thai patients find it easier to get used to certain chronic health conditions, and let them go easier, because of the cultural and spiritual beliefs of this region. This may be why our control group performed well with general tinnitus management relative to the MBCT group. The results of this study indicate that MBCT is feasible in Thai individuals, even for shorter periods of initial practice, and suggest that it can be used as a component of integrative therapy in patients with chronic tinnitus.
Further studies are needed to identify optimal combinations of available treatment methods for tinnitus patients according to the tinnitus cause and development of symptoms. Further, future studies with larger populations and longer follow-up periods are needed to compare the cost-effectiveness of MBCT and other treatments, with the aim of developing guidelines for treating tinnitus and improving the quality of life of patients.
Study Limitations
This study had some limitations. First, this was a quasiexperimental study without randomization. However, the demographic data and baseline characteristics between the groups were not different. This study was non-blinded because of the nature of the intervention. Second, some participants also received other treatments, such as medication, acupuncture, and hearing aids. These confounding variables were unavoidable. However, these factors did not differ between the groups. As mentioned, studies with larger sample sizes, longer periods of practice, and longer follow-up periods are needed.
Conclusion
This study revealed that MBCT was effective in improving the quality of life in patients with tinnitus. MBCT is feasible in Thai patients, has no harmful effects, is easily accessible, and is low cost. Thus, it should be considered as an additional treatment option for patients with tinnitus.
Acknowledgements
We appreciate the cooperation of all our participants throughout the study. We would like to express our gratitude to assistant professor Dr. Alongkot Emmasith for her recommendation and preparation of the English manuscript, and to associate professor Dr. Chatchawan Silpakit, a well-known psychiatrist, who has practiced mindfulness for more than ten years. At the time of this study, he was the director of the Contemplation Education Center at Mahidol University. We thank Sydney Koke, MFA, from Edanz (https://www.edanz.com/ac) for editing a draft of this manuscript. We declared of no conflicting interests and no funding need because the mindfulness meditation is free for all mankind.
References
- Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham Jr ER, et al. Clinical practice guideline: tinnitus. Otolaryngol–Head and Neck Surg. 2014;151(2):S1-40.
- Heller AJ. Classification and epidemiology of tinnitus. Otolaryngologic Clinics of North America. 2003;36(2):239-48.
- Adrian D, El Refaie A. The epidemiology of tinnitus. In The handbook of tinnitus 2000:1-23.
- Oosterloo BC, Croll PH, Baatenburg de Jong RJ, Ikram MK, Goedegebure A. Prevalence of tinnitus in an aging population and its relation to age and hearing loss. Otolaryngol–Head and Neck Surg. 2021;164(4):859-68.
- Axelsson A, Ringdahl A. Tinnitus—a study of its prevalence and characteristics. British J Audiol. 1989;23(1):53-62.
- Lewis JE, Stephens SD, McKenna L. Tinnitus and sucide. Clinical Otolaryngol & Allied Sci. 1994;19(1):50-4.
- Gold JR, Bajo VM. Insult-induced adaptive plasticity of the auditory system. Front in Neurosci. 2014;8:110.
- Auerbach BD, Rodrigues PV, Salvi RJ. Central gain control in tinnitus and hyperacusis. Front in Neurol. 2014;5:206.
- Newman CW, Jacobson GP, Spitzer JB. Development of the tinnitus handicap inventory. Arch of Otolaryngol–Head & Neck Surg. 1996;122(2):143-8.
- Siriporn Limviriyakul MD, Supavanich W. The validity and reliability of tinnitus handicap inventory Thai version. J Med Assoc Thai. 2012;95(11):1433-40.
- Andersson G, Porsaeus D, Wiklund M, Kaldo V, Christian Larsen H. Treatment of tinnitus in the elderly: A controlled trial of cognitive behavior therapy: Tratamiento del acúfeno en ancianos: una prueba controlada de terapia conductual cognitiva. Int J Audiol. 2005;44(11):671-5.
- Jastreboff PJ, Hazell JW. Tinnitus retraining therapy: Implementing the neurophysiological model. Cambridge University Press; 2008.
- Hoare DJ, Kowalkowski VL, Kang S, Hall DA. Systematic review and meta-analyses of randomized controlled trials examining tinnitus management. The Laryngoscope. 2011;121(7):1555-64.
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192-217.
- Kiecolt-Glaser JK, Page GG, Marucha PT, MacCallum RC, Glaser R. Psychological influences on surgical recovery: perspectives from psychoneuroimmunology. Am Psychol. 1998;53(11):1209.
- Salovey P, Rothman AJ, Detweiler JB, Steward WT. Emotional states and physical health. Am Psychol. 2000;55(1):110.
- Londero A, Peignard P, Malinvaud D, Nicolas-Puel C, Avan P, Bonfils P. Contribution of cognitive and behavioral therapy for patients with tinnitus: implication in anxiety and depression. InAnnales d'oto-laryngologie et de chirurgie cervico faciale: Bulletin de la Societe d'oto-laryngologie des hopitaux de Paris 2004;121(6):334-345.
- Cima RF, Maes IH, Joore MA, Scheyen DJ, El Refaie A, Baguley DM, et al. Specialised treatment based on cognitive behaviour therapy versus usual care for tinnitus: A randomised controlled trial. The Lancet. 2012;379(9830):1951-9.
- Thompson DM, Hall DA, Walker DM, Hoare DJ. Psychological therapy for people with tinnitus: A scoping review of treatment components. Ear and Hearing. 2017;38(2):149.
- Martinez-Devesa P, Waddell A, Perera R, Theodoulou M. Cognitive behavioural therapy for tinnitus. Cochrane Database of Systematic Rev. 2007(1).
- Peterson LG, Pbert L. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149(7):936-43.
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. Jama. 2008;300(11):1350-2.
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. J Consulting and Clin Psychol. 2002;70(2):275.
- Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Med. 2003;65(4):564-70.
- Sadlier M, Stephens SD, Kennedy V. Tinnitus rehabilitation: a mindfulness meditation cognitive behavioural therapy approach. The J Laryngol & Otol. 2008;122(1):31-7.
- Roland LT, Lenze EJ, Hardin FM, Kallogjeri D, Nicklaus J, Wineland AM, et al, Effects of mindfulness based stress reduction therapy on subjective bother and neural connectivity in chronic tinnitus. Otolaryngol--Head and Neck Surg. 2015;152(5):919-26.
- Philippot P, Nef F, Clauw L, de Romrée M, Segal Z. A randomized controlled trial of mindfulness-based cognitive therapy for treating tinnitus. Clin Psychol & Psychother. 2012;19(5):411-9.
- Kreuzer PM, Goetz M, Holl M, Schecklmann M, Landgrebe M, Staudinger S, et al. Mindfulness-and body-psychotherapy-based group treatment of chronic tinnitus: a randomized controlled pilot study. BMC Complementary and Alternative Med. 2012;12(1):1-8.
- McKenna L, Marks EM, Hallsworth CA, Schaette R. Mindfulness-based cognitive therapy as a treatment for chronic tinnitus: a randomized controlled trial. Psychother and Psychosomatics. 2017;86(6):351-61.
- Arif M, Sadlier M, Rajenderkumar D, James J, Tahir T. A randomised controlled study of mindfulness meditation versus relaxation therapy in the management of tinnitus. The J Laryngol & Otol. 2017;131(6):501-7.
- Areekit P, Lueboonthawatchai O. The effect of cognitive and behavioral therapy program together with mindfulness on depression in depressed patients. J Psychiatr Nurs Mental Health. 2012;26(3),71-80.
- Lortrakul M. Editorial Handbook for mental health and psychiatric care for doctors. Revised 1st edition. Bangkok: Department of Mental Health, MPH. 2001:308-13.
- McKenna L, Marks EM, Vogt F. Mindfulness-based cognitive therapy for chronic tinnitus: Evaluation of benefits in a large sample of patients attending a tinnitus clinic. Ear and Hearing. 2018;39(2):359-66.
- Rademaker MM, Stegeman I, Ho-Kang-You KE, Stokroos RJ, Smit AL. The effect of Mindfulness-Based interventions on tinnitus distress. A systematic review. Front in Neurol. 2019:1135.
- Husain FT, Zimmerman B, Tai Y, Finnegan MK, Kay E, Khan F, et al. Assessing mindfulness-based cognitive therapy intervention for tinnitus using behavioural measures and structural MRI: A pilot study. Int J Audiol. 2019;58(12):889-901.
- Martinez-Devesa P, Waddell A, Perera R, Theodoulou M. Cognitive behavioural therapy for tinnitus. Cochrane Database of systematic Rev. 2007(1).
- Marks E, Smith P, McKenna L. I wasn’t at war with the noise: How mindfulness based cognitive therapy changes patients’ experiences of tinnitus. Front in Psychol. 2020;11:483.
- Marks E, Smith P, McKenna L. Living with tinnitus and the health care journey: An interpretative phenomenological analysis. British J Health Psychol. 2019;24(2):250-64.
- Ogawa K, Sato H, Takahashi M, Wada T, Naito Y, Kawase T, et al. Clinical practice guidelines for diagnosis and treatment of chronic tinnitus in Japan. Auris Nasus Larynx. 2020;47(1):1-6.
- National Institute for Health and Care Excellence Tinnitus: assessment and management. NICE Guideline [155].2020:11.
- Jayasaro A. Without and within: Questions and answers on the teachings of Theravada Buddhism. Buddhadasa Indapanno Arch; 2013.
Department of Otolaryngology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Send correspondence to:
Chanchai Jariengprasert
Department of Otolaryngology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Tel: 0859221122
E-mail: chanchai.jar@mahidol.ac.th
Paper submitted on February 01, 2022; and Accepted on February 18, 2022
Citation: Chanchai Jariengprasert, Kasinee Watanapornmongkol, Sivaporn Kiatthanabumrung, Tosapohn Wisupagan. The Effectiveness of Mindfulness-Based Cognitive Therapy in the Management of Tinnitus. 2022;26(1):1-10