The International Tinnitus Journal
Official Journal of the Neurootological and Equilibriometric Society
Official Journal of the Brazil Federal District Otorhinolaryngologist Society
ISSN: 0946-5448

Google scholar citation report
Citations : 12717
The International Tinnitus Journal received 12717 citations as per google scholar report
The International Tinnitus Journal peer review process verified at publons
Indexed In
- Excerpta Medica
- Scimago
- SCOPUS
- Publons
- EMBASE
- Google Scholar
- Euro Pub
- CAS Source Index (CASSI)
- Index Medicus
- Medline
- PubMed
- UGC
- EBSCO
Volume 27, Issue 2 / December 2023
Research Article Pages:191-197
10.5935/0946-5448.20230029
The Rate of Cesarean Section and Newborn Apgar score In Two Types Of Physiological Delivery and Facilitated Delivery in Mothers with First Pregnancy
Authors: Tiba Mirzarahimi, Faranak Jalilvand*, Khatereh Isazadehfar, Farinaz Babazadeh Nanekaran
PDF
Abstract
Introduction: Labor pain is often severe and its lack of relief can have a bad effect on the mother's physiological condition. Accurate measurement and appropriate treatment of pain is an important problem. There are several choices for the control of labor pain, however, each method has its own risks and benefits regarding its efficiency and availability; therefore, the aim of this study was to compare the rate of cesarean section and newborn Apgar in two types of physiological delivery and facilitated delivery among mothers with first delivery. Materials and methods: This case-control study was conducted on mothers aged 18-35 who went to the hospital to give birth. In the present study, 8 sessions (90 minutes each session) were held to prepare mothers from 20 to 37 weeks of pregnancy. Candidate mothers for physiological labor were hospitalized without intervention and in the active phase of labor, and their labor stages were planned physiologically. The pain intensity of mothers was asked using a scale (VAS) during labor every half hour (according to the pain scale from 0 to 10). The average score of pain during the first and second stages, type of delivery, amount of postpartum bleeding, length of the stage of delivery, infection, and fever after delivery, Apgar score of the baby, perineal status, mother's satisfaction and the rate of hospitalization of the baby in NICU were recorded. Furthermore, the level of satisfaction with childbirth was evaluated with the help of Mackey's standard satisfaction questionnaire. Results: The average age of the physiological delivery and facilitated delivery groups was 26.37 ± 5.23 years and 26.58 ± 5.79 years, respectively. Physiological delivery significantly required less conversion to cesarean section. The most common etiology was caesarean section in the physiologic labor group, and a drop in NST was reported in the facilitated group. The analysis of the results demonstrated no significant difference between the etiology of cesarean section and the study groups. The Apgar score in the physiological group was significantly better than the facilitated group. There is no significant relationship between the study group and the amount of bleeding during delivery. Furthermore, there was no significant relationship between the study group and the incidence of postpartum infection. The rate of NICU admission in the facilitated group was found to be significantly higher than physiological delivery. Conclusion: The results of this study revealed that the rate of caesarean section, the rate of need for NICU, newborns' Apgar score, and the rate of mothers' satisfaction in physiological delivery group were significantly different from the other groups, but the rate of wound infection and the amount of postpartum bleeding in the two groups showed a significant difference.
Keywords: Cesarean section, Newborn Apgar, Physiological delivery, Facilitated delivery, Mothers with first pregnancy.
Introduction
Childbirth is a phenomenon during which the beginning of labor contractions leads to delivery and the removal of the placenta [1]. Pain during childbirth and pregnancy is caused by uterine contractions, dilation of the cervix and expansion of the perineum [2]. The intensity of labor pains and its long duration is one of the most important factors encouraging pregnant women towards cesarean delivery, which not only requires more specialized facilities and higher costs, but also creates more complications for the mother. Childbirth pain is one of the excruciating pains that women experience during their lifetime [3]. This pain is more intense and longer especially in the first delivery. Several studies have only compared pain caused by amputation and myocardial ischemia [4].
Pain is an unpleasant feeling that medical science has always tried to eliminate or reduce [5]. However, the intensity and level of pain tolerance varies among people under different conditions [6]. According to the studies, 77% of first births result in severe and unbearable labor pain [7]. Childbirth pain can cause several adverse effects on the birth process, and the state of the mother and the fetus. The severe pain of childbirth may create long-term emotional imbalances and disturb the mental health of the mother, which has a negative effect on the important relationship between the mother and the baby in the first days of life [8]. Unwanted symptoms caused by labor pain in the fetus, including: late drop in heart rate, decrease in maternal arterial oxygen pressure, decrease in uteroplacental blood flow due to severe contraction of the uterus during labor pain and fetal acidosis in some of the cases [9]. Therefore, it seems necessary to evaluate cheap methods with fewer side effects for the mother and the baby that require less use of specialized personnel in this field. Today, there are many methods and medicines that can eliminate or reduce the intensity of labor pain [10]. All these methods are divided into four groups: psychological methods, drug methods, local painkillers and inhalation anesthetics [11]. Pharmacological measures are usually effective but often have harmful effects. Medicinal methods only eliminate the physical sense of pain, while non-medicinal methods prevent mothers from suffering during childbirth by improving the psychological and emotional aspects of childbirth [12].
The rate of cesarean section in Iranian mothers is high and the importance of facilitated delivery is very important to encourage women to do it, but sufficient information about maternal and neonatal complications in facilitated delivery is needed. Therefore, the purpose of this study is to compare the rate of cesarean section and Apgar score of the newborn in two types of physiological delivery and facilitated delivery in mothers with the first pregnancy.
Therefore, this study aimed at comparing the rate of cesarean section and Apgar scores of newborns in two types of physiological delivery and facilitated delivery in mothers with the first pregnancy.
Materials and Methods
This case-control study was conducted on 18-35-year-old first-term mothers who visited Alavi Hospital in Ardabil-Iran from March 2020 to March 2021. Pregnant women were included in the study by census, and patients who met the inclusion and exclusion criteria were included in the study. Inclusion criteria included: singleton pregnancy, no bad obstetric or medical history, no drug or addiction use, willingness to have a natural birth, having a BMI of 20-30, no underlying disease. Exclusion criteria included: medical or obstetric complications during pregnancy such as hypertension, diabetes, bleeding and preterm delivery, rupture of the water sac for more than 24 hours, mothers with a large fetus, BMI below 20 and above 30, and lack of consent to participate in the study. There were about 200 patients who were divided into two control and case groups.
Procedure
At first, mothers were prepared for childbirth from the 20th to the 37th week of pregnancy during 8 sessions (90 minutes each session). In these meetings, explanations were given about the process of labor, methods of reducing the pain and analgesia of childbirth, pregnancy changes, personal and nutritional care, increasing the awareness of family members, especially the father, regarding changes during pregnancy, newborn health, breastfeeding and mother support.
Training during childbirth including breathing techniques, relaxed body and perineum based on kinesiology, labor and delivery positions, correction of pregnancy positions and skeletal muscle exercises, refraining from actions such as fasting of the mother, taking veins, limiting the movement of the mother during labor, giving birth by lithotomy, induction, episiotomy.
Candidate mothers for physiological labor were hospitalized in the active phase of labor without intervention and their labor stages were planned physiologically. Vaginal examinations were performed every 2 hours and FHR every half hour in the first stage and every quarter hour in the second stage. During the stages of labor, liquids were consumed within the allowed limit.
Candidate mothers were admitted for facilitated delivery according to the emergency method (in latent or active phase) and were controlled according to the routine of the delivery room, i.e., venipuncture, augmentation, monitoring and hourly examinations. During delivery, episiotomy was not routinely used in the physiological delivery method. In the case of a relatively large fetus, a hard perineum episiotomy was given and the patient had the pushing phenomenon according to the intensity of the pain and his own desire.
The pain intensity of mothers was asked using a scale (VAS) during labor every half hour (according to the pain scale from 0 to 10). The average score of pain during the first and second stage, type of delivery, amount of postpartum bleeding, length of the stage of delivery, infection and fever after delivery, Apgar score of the baby, perineal status, mother’s satisfaction and the rate of hospitalization of the baby in NICU were recorded. Furthermore, the level of satisfaction with childbirth was evaluated with the help of Mackey’s standard satisfaction questionnaire.
Data analysis
Central indices (mean, median, etc.) and dispersion indices (standard deviation, variance, etc.) were used to analyze descriptive information. T and Chi-square statistical tests were used in this study. SPSS software was used for data analysis. A significance level of 0.05 was considered for all tests.
Ethical considerations
The information of all the patients was kept confidential. This study was performed in accordance with relevant regulations in the ethics research committees of the University of Medical Sciences and Declaration of Helsinki. The project was carried out after being approved by the Research Council of the Faculty of Medicine.
Results
A total of 200 pregnant women candidates for natural delivery in two groups of physiological delivery and facilitated delivery were included in the study. The average age of the physiological delivery and facilitated delivery groups was 26.37 ± 5.23 years and 26.58 ± 5.79 years, respectively (P=0.788). Also, the physiological delivery group had 35 mothers in the age range of 26-30 years, and the facilitated delivery group had 33 mothers in the age range of 21-25 years (P=0.788) Figure 1.
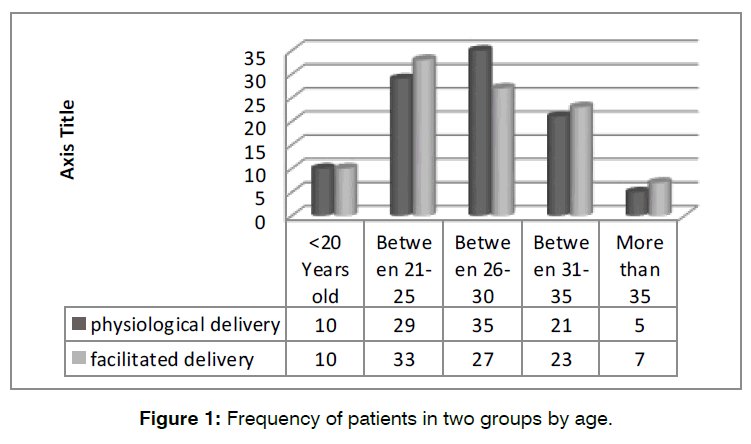
Figure 1: Frequency of patients in two groups by age.
The need for cesarean section of both delivery methods was compared. If the mothers had indications for cesarean section, they entered the cesarean phase and NVD (Normal Vaginal Delivery) delivery was replaced by cesarean section. The results of this study demonstrated that 21 mothers (21%) in the facilitated delivery group and 3 mothers (3%) in the physiological delivery group underwent cesarean section. The findings revealed that physiological delivery was significantly less likely to require cesarean delivery (P=0.000) Figure 2.
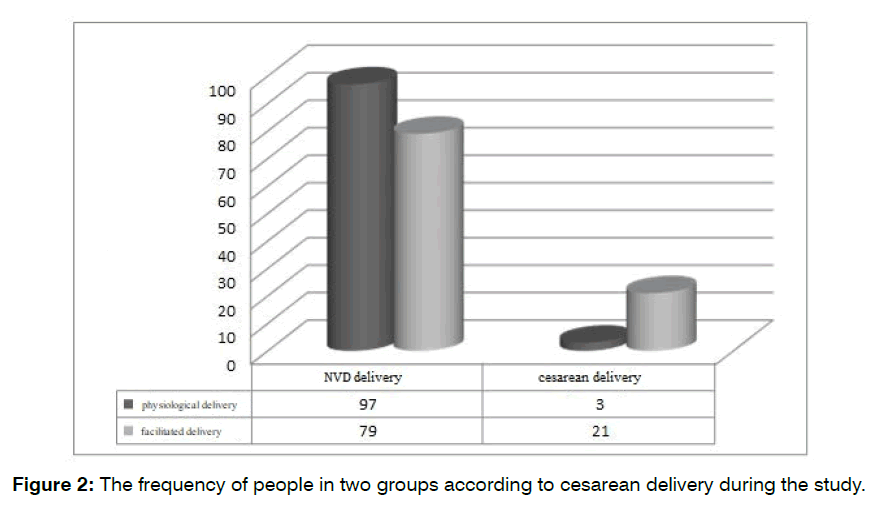
Figure 2: The frequency of people in two groups according to cesarean delivery during the study.
In Table 1, the etiology of caesarean section during the natural childbirth process of mothers is shown. The most common etiology of caesarean section was observed in the physiological delivery group. A decrease in NST was reported in the facilitated group. The analysis of the results showed no significant difference between the etiology of cesarean section and the study groups (P=0.057).
| Physiological group | facilitated group | ||||
|---|---|---|---|---|---|
| Etiology of cesarean section | Frequency | Percent | Frequency | Percent | P value |
| Delivery stop | 3 | 100 | 6 | 28.6 | 0.057 |
| Meconium discharge | 0 | 0 | 3 | 14.3 | |
| NST drop | 0 | 0 | 12 | 57.1 | |
Table 1: Frequency of caesarean section etiology by groups.
The Apgar score of babies after birth is also shown in Table 2. The results showed that all babies in the physiological group had an Apgar score of 9 after birth, but only 78 babies in the facilitated group had such an Apgar score after birth. The analysis of the results demonstrated that the Apgar score in the physiological group was significantly better than the facilitated group (P=0.000).
| physiological group | facilitated group | ||||
|---|---|---|---|---|---|
| Apgar of newborns | Frequency | Percent | Frequency | Percent | P value |
| 9 | 100 | 100 | 78 | 78 | 0.000 |
| 8 | 0 | 0 | 21 | 21 | |
| 7 | 0 | 0 | 1 | 1 | |
Only 3 mothers in the facilitated delivery group had more than 500cc of bleeding. Other patients showed bleeding less than 500cc. There is no significant relationship between the study group and the amount of bleeding during delivery (P=0.081). Postpartum infection was also investigated in both groups. The results showed that only one patient (1%) in the facilitated delivery group had a postpartum infection, where no statistically significant relationship between the study group and the incidence of postpartum infection (P=0.316).
Table 3 shows the relationship of patients with pain who underwent natural delivery. The results showed that all the mothers in the physiological delivery group had a pain score of 9-10. Meanwhile, 65 mothers (83.3%) in the facilitated delivery group mentioned such pain. The results showed a statistically significant relationship between pain intensity and study groups (P=0.000).
| physiological group | facilitated group | ||||
|---|---|---|---|---|---|
| Intensity of pain | Frequency | percent | Frequency | percent | P value |
| 9-10 | 97 | 100 | 65 | 82.3 | 0.000 |
| 7-8 | 0 | 0 | 14 | 17.7 | |
The frequency of patients in two groups was analyzed according to the satisfaction of the patients with childbirth Figure 3. According to the results, 52 mothers (52%) of the physiological group and 65 mothers (65%) of the facilitated group have chosen a good level of satisfaction for their delivery.
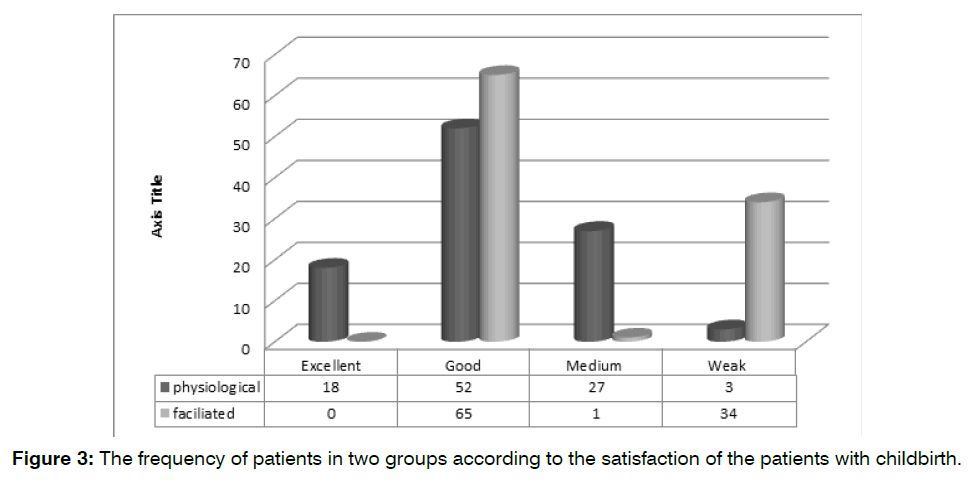
Figure 3: The frequency of patients in two groups according to the satisfaction of the patients with childbirth.
The results showed that 12 babies in the facilitated delivery group had NICU admission after birth. Analysis of the results revealed that the rate of NICU admission in the facilitated group was significantly higher than physiological delivery (P=0.000).
Discussion
The increase in cesarean delivery rates has been a concern, especially in developed countries [13]. In a systematic review and meta-analysis on 197,514 pregnant women, the prevalence of cesarean delivery in Iran was estimated at 48% [14]. The prevalence of cesarean in Ireland, the United States of America, and Brazil was 31.3, 31.6, and 48.4%, respectively [15]. Therefore, the aim of this study was to compare the rate of cesarean section and Apgar scores of newborns in two types of physiological delivery and facilitated delivery in mothers with first pregnancy.
In this study, the majority of patients were in the age range of 21-30 years and their average age was around 26 years. Sehati et al.’s study [16] on 370 primiparous mothers showed that the average age of mothers in the physiological delivery group and the facilitated delivery group were 23.17 and 22.72 years, respectively. Haratipour et al. [17] reported that the average age of mothers in the physiological group and the facilitated group was 27.56 years and 26.21 years, respectively. In Oshvandi et al.’s study [18], the average age of mothers in the physiological vaginal group and the facilitated delivery group was 27.7 and 27.37 years, respectively. The average age of the majority of studies is similar to each other, indicating the use of younger mothers in the majority of studies.
Physiological delivery significantly reduced the need for cesarean section (P<0.001), but the rate of infection after surgery (P=0.316) was not significantly different between the two groups. In Sehati et al.’s study (16), it was also observed that the rate of cesarean section following facilitated delivery in primiparous women is more than women with physiological delivery (P<0.001). Gerber et al.’s study [19] reported that the facilitated delivery group had a significantly increased risk of cesarean section and fetal membrane infections compared to the physiologic delivery group.
The study of Van Gemund et al. [20] showed that the cesarean rate in the facilitated labor group was higher than in the physiological labor group and without manipulation due to the lack of labor progress and fetal heart rate drop. In physiological delivery, there was no intervention on the patients and there were fewer disturbances in the delivery process of the mothers; so, probably for this reason, the rate of caesarean section during delivery in people with physiological delivery is significantly lower than the other group.
In this study, the amount of postpartum bleeding (within 6 hours) did not show a significant difference in the two groups (P=0.081). Oshvandi et al.’s study [18] examined the average hemoglobin in 6 hours after delivery with the previous stage in physiological and facilitated delivery where this average decreased significantly over time in both groups. In other words, the amount of hemoglobin drop was significant in both groups, but the two groups did not show a significant difference 6 hours after delivery. Osmundson et al.’s study [21] revealed that the rate of postpartum bleeding in the physiological delivery group and the facilitated delivery group was 3.4% and 4.1%, although this rate was less in the spontaneous delivery group, a statistically significant difference was found between the two groups. The results of the study by Buzaglo [22] and Sheiner [23] showed that induction with oxytocin can lead to postpartum hemorrhage and a drop in hemoglobin and hematocrit after delivery. The cause of this bleeding after induction with oxytocin is the increased risk of uterine atony, which has been suggested as the main cause of decreased sensitivity of uterine receptors to oxytocin.
The study of Van Gemund and colleagues [20] was conducted on two groups of physiological labor and facilitated labor to investigate amount of interventions during labor, where the amount of sedation, delivery with episiotomy, pressure on the fundus for faster head exit in the second stage of labor, use of oxytocin and metrogen group increased significantly. Contrary to these results, a study by Dolatian et al. [24] compared the effect of three methods of using Syntometrine, Syntocinon and physiological management of the third stage of labor and concluded that the amount of bleeding was more and the amount of hematocrit was less in the group of physiological management of the third stage than two other groups.
Non-interference during labor in mothers such as avoiding episiotomy or using different drugs can be a reason for reducing bleeding in mothers undergoing physiological labor, which was confirmed in the majority of studies, but was not observed in the present study. This reason was probably due to improper and inaccurate measurement of bleeding and the lack of using hemoglobin and hematocrit levels for bleeding in mothers.
In this study, the Apgar score of the newborns was better in the physiological delivery group than in the facilitated group. In Sehati et al.’s study [16], no statistically significant difference was found between the two delivery groups in the Apgar of the first minute of the baby at the time of birth (P=0.32), but there was a significant statistical difference in the Apgar of the fifth minute after delivery, where the average Apgar of 9.8 and 9.52 were obtained for the physiological delivery group and the facilitated delivery group (P<0.001). Cheng et al.’s study [25] revealed that with the increase in the duration of the second stage of labor, the birth of a baby with an Apgar score of less than 7, the need to resuscitate the baby, and the pH of the umbilical cord blood in the group of physiological delivery is significantly lower than that of facilitated delivery.
In Gerber et al.’s study19, it was also observed that the Apgar score of the fifth minute in primiparous babies had a statistically significant difference between the two groups, so that the Apgar score in babies with physiological delivery was significantly higher than that of babies undergoing facilitated delivery. P<0.001). In Oshvandi et al.’s study [18], the comparison of the Apgar scores of infants in the two groups of physiological and facilitated delivery at the first and fifth minute also showed that the Apgar score in the physiological delivery group was higher than that of the facilitated vaginal delivery (P<0.05). Jahadi [26] and Rahimikian [27] observed that the Apgar score of the newborns in minutes one and five in the physiological delivery group was significantly higher than the facilitated group. A better birth event and avoiding interference in childbirth can lead to childbirth and the birth of babies with a better Apgar score, which is probably due to the natural process of childbirth and its non-acceleration and the development of the baby during the delivery process. This finding was confirmed in the majority of studies and consistent with the present study.
In this study, mothers’ satisfaction with physiological delivery was significantly higher than the facilitated delivery group Jafari et al. [28] showed that mothers were highly satisfied with the delivery environment in both facilitated and physiological delivery groups, where none of the two groups included people in the “dissatisfied” and “very dissatisfied” categories.
More than 92.4% of mothers in the physiological delivery group were “very satisfied” with the delivery environment. While in the facilitated delivery group, 58.2% were fully satisfied (P<0.0001). Also, 76.8% of physiological birth mothers and 40.7% of facilitated birth mothers were fully satisfied with the birth experience (P=0.001). Physiological delivery was able to create an acceptable percentage of satisfaction in mothers. Shakri et al. [29] observed that the average anxiety of mothers at the beginning of the delivery process in the two groups of physiological delivery and the facilitated method did not show a significant difference, but it reduced the amount of maternal anxiety during the continuation of the delivery process and managing the delivery process by the physiological method with a minimum Interventions.
It was also observed that in the physiological delivery group, 27% of the research units were satisfied with the process of labor and delivery and after delivery, but 14% of the mothers with the normal delivery were satisfied with the delivery process in the facilitated delivery group.
The results of the research showed a significant difference between the two studied groups in terms of the level of satisfaction in the two studied groups (P=0.001). Heratipour et al. [17] observed that the mothers of the physiological delivery group had a higher level of attachment to their babies than the other group. However, no statistically significant difference was observed in terms of the amount of stress and anxiety in the two groups. Due to the fact that physiological birth involves the least interventions on the mother, establishment of the balance in the mother’s hormonal system and less adrenaline level, as a result, fear and anxiety are reduced and labor progresses well. It can be expected that the neonatal outcomes in mothers who give birth by physiological methods are better than mothers who give birth by conventional or facilitated methods.
In this study, it was observed that the admission rate of newborns after delivery in the NICU department was significantly higher in the facilitated group than in the physiological group. Oshvandi et al. [28] reported that none of the infants in the two study groups required hospitalization in the NICU.
Conclusion
The results of this study showed that the rate of caesarean section, the rate of need for NICU, Apgar of newborns, and the rate of mothers’ satisfaction with physiological delivery had a significant difference with the other groups, but the rate of wound infection and the amount of postpartum bleeding did not show a significant difference in the two groups.
References
- Yilmaz EA, Gülümser Ç. The risk factors, consequences, treatment, and importance of gestational depression. Turk J Obstet Gynecol. 2015;12(2):102.
- Ancel J, Rault E, Fernandez MP, Huissoud C, Savidan A, Gaire C, et al. When can obstetric risk be predicted?. J Gynecol Obstet Hum. 2019 ;48(3):179-86.
- Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017;317(21):2207-25.
- Barlow J, Smailagic N, Huband N, Roloff V, Bennett C. Group-based parent training programmes for improving parental psychosocial health. Campbell Syst Rev. 2012;8(1):1-97.
- Kamali A, Azadfar R, Pazuki S, Shokrpour M. Comparison of dexmedetomidine and fentanyl as an adjuvant to lidocaine 5% for spinal anesthesia in women candidate for elective caesarean. Open Access Maced J Med Sci. 2018;6(10):1862.
- Moshiri E, Modir H, Kamali A, Azami M, Molouk M. Comparative analgesic, hemodynamic, pain and duration of sensory and motor block effects of dexmedetomidine, granisetron, and nitroglycerin added to ropivacaine in intravenous anesthesia for forearm surgeries: a randomized clinical study. Med Gas Res. 2022;12(3):77.
- Pinar G, Avsar F, Aslantekin F. Evaluation of the impact of childbirth education classes in Turkey on adaptation to pregnancy process, concerns about birth, rate of vaginal birth, and adaptation to maternity: a case-control study. Clin Nurs Res. 2018;27(3):315-42.
- Merzougui L, Marwen N, Hannachi H, Asma M, Elhaj OB, Waddah M, et al. Incidence and risk factors of surgical site infection following caesarean section in a Tunisian maternity unit. Can J Public Health. 2018;30(3):339-47.
- Naemi AR, Kashanitabar V, Kamali A, Shiva A. Comparison of the effects of haloperidol, metoclopramide, dexmedetomidine and ginger on postoperative nausea and vomiting after laparoscopic cholecystectomy. J Med Life. 2020;13(2):206.
- Brixval CS, Axelsen SF, Lauemøller SG, Andersen SK, Due P, Koushede V. The effect of antenatal education in small classes on obstetric and psycho-social outcomes-a systematic review. Syst Rev. 2015;4(1):1-9.
- Spong CY, Cunningham F, Leveno K, Bloom S, Hauth J, Rouse D. Williams obstetrics. New York: McGraw-Hill Education. 2009.
- Yildirim D, Ozyurek SE, Ekiz A, Eren EC, Hendem DU, Bafali O, et al. Comparison of active vs. expectant management of the third stage of labor in women with low risk of postpartum hemorrhage: a randomized controlled trial. Ginekol Pol. 2016;87(5):399-404.
- Vogel JP, Betrán AP, Vindevoghel N, Souza JP, Torloni MR, Zhang J, et al. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Health. 2015;3(5):e260-70.
- Rafiei M, Ghare MS, Akbari M, Kiani F, Sayehmiri F, Sayehmiri K, et al. Prevalence, causes, and complications of cesarean delivery in Iran: A systematic review and meta-analysis. Int J Reprod Biomed. 2018;16(4):221.
- Hehir MP, Ananth CV, Siddiq Z, Flood K, Friedman AM, D’Alton ME. Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-Group Classification System. Am J Obstet Gynecol. 2018;219(1):105-e1.
- Sehhati Shafai F, Kazemi S. Comparing maternal outcomes in nulliparous women in labor in physiological and conventional labor: a randomized clinical trial. J Maz Univ Med. 2013;22(97):122-31.
- Haratipour H, Partash N, Ebrahimi E, Zadeh MD, Bolbolhaghighi N. Non-physiological and physiological delivery method: comparison of maternal attachment behaviors and anxiety. J Caring Sci. 2021;10(1):37.
- Oshvandi K, Masoumi SZ, Kazemi F, Shayan A, Oliaei SS, Mohammadi A. Comparison of Maternal Anemia and Their Infant Apgar Scores in Conventional Vaginal Delivery with Physiological Delivery. Avicenna J Med Biotechnol. 2020;28(4):9-19.
- Gerber S, Vial Y, Hohlfeld P. Maternal and neonatal prognosis after a prolonged second stage of labor. J Gynecol Obstet Biol Reprod. 1999;28(2):145-50.
- Van Gemund N, Hardeman A, Scherjon SA, Kanhai HH. Intervention rates after elective induction of labor compared to labor with a spontaneous onset: a matched cohort study. Gynecol Obstet Invest. 2003;56(3):133-8.
- Osmundson S, Ou-Yang RJ, Grobman WA. Elective induction compared with expectant management in nulliparous women with an unfavorable cervix. Obstet Gynecol. 2011;117(3):583-7.
- Buzaglo N, Harlev A, Sergienko R, Sheiner E. Risk factors for early postpartum hemorrhage (PPH) in the first vaginal delivery, and obstetrical outcomes in subsequent pregnancy. J Matern Fetal Neonatal Med. 2015;28(8):932-7.
- Sheiner E, Sarid L, Levy A, Seidman DS, Hallak M. Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Matern Fetal Neonatal Med. 2005;18(3):149-54.
- Dolatian M, Shademan N. Efficacy of syntometrine, syntocinon and the physiologic approach in the management of the third stage of labor. Med Res J. 2003;27(3):191-6.
- Cheng YW, Delaney SS, Hopkins LM, Caughey AB. The association between the length of first stage of labor, mode of delivery, and perinatal outcomes in women undergoing induction of labor. Am J Obstet Gynecol. 2009;201(5):477-e1.
- Jahdi F, Shanazari Avag M, Kashanian M, Ashgehi Farahani M, Hagani H. The effect of physiological birth in outcomes of delivery. Tehran university. 2009.
- Rahimikian F, Talebi F, Golian Tehrani S, Mehran A. Comparison of the effect of physiological birth and routine normal delivery on some of maternal and fetus outcomes. J Ardabil Univ Med Sci. 2013;13(4):398-405.
- Jafari A, Mohebi P, Rostagari L, Mazloumzadeh S. A comparative study of the level of satisfaction of mothers in giving birth by the physiological method with the conventional method in Ayatollah Mousavi Hospital, Zanjan. Iran J Obstet Gynecol Infertil. 2013; 16(73): 9-18.
- Shakri M, Mohammadian F, Shahnawaz A, Sarmi F. Comparison of anxiety and satisfaction of primiparous women in two methods of physiological and conventional delivery. J Babol Univ Medical Sci. 2013; 5(4): 42-49.
1Department of Obstetrics and Gynecology, Alavi Hospital, Ardabil University of Medical Science, Ardabil, Iran
2Infertility Fellowship, Ardabil University of Medical Science, Ardabil, Iran
3Determinants of Health Research Center, Department of Community Medicine, School of Medicine, Ardabil University of Medical Sciences, Ardabil, Iran
4Department of Obstetrics and Gynecology, Ardabil University of Medical Science, Ardabil, Iran
Send correspondence to:
Faranak Jalilvand
Infertility Fellowship, Ardabil University of Medical Science, Ardabil, Iran, E-mail: faranjalili@gmail.com
Paper submitted on October 27, 2023; and Accepted on November 17, 2023
Citation: Jalilvand F. The Rate of Cesarean Section and Newborn Apgar score In Two Types Of Physiological Delivery and Facilitated Delivery in Mothers with First Pregnancy. Int Tinnitus J. 2023;27(2):191-197.


